Acute and Chronic Liver Disease: Detailed Overview
The liver is a vital organ responsible for various functions, including detoxification, protein synthesis, and bile production. Liver disease encompasses a range of conditions that affect the liver’s function and structure. These can be classified into acute and chronic liver diseases based on their duration and progression.
Acute Liver Disease
Definition: Acute liver disease, also known as acute liver failure, is a rapid deterioration of liver function that occurs within days to weeks. It is characterised by jaundice, coagulopathy (blood clotting abnormalities), and encephalopathy (brain dysfunction).
Causes:
- Viral Hepatitis: Hepatitis A, B, and E are common viral causes.
- Drug-Induced Liver Injury: Overdose or adverse reactions to drugs such as paracetamol (acetaminophen).
- Toxins: Ingestion of toxic substances like certain mushrooms or industrial chemicals.
- Autoimmune Hepatitis: The immune system attacks liver cells.
- Vascular Disorders: Conditions such as Budd-Chiari syndrome (blockage of hepatic veins).
Symptoms:
- Jaundice: Yellowing of the skin and eyes due to elevated bilirubin.
- Encephalopathy: Confusion, altered consciousness, and coma.
- Coagulopathy: Increased tendency to bleed due to impaired synthesis of clotting factors.
- Abdominal Pain: Particularly in the upper right quadrant.
- Nausea and Vomiting: General digestive discomfort.
Diagnosis:
- Blood Tests: Liver function tests (ALT, AST, bilirubin), coagulation profile (INR), and tests for viral hepatitis.
- Imaging Studies: Ultrasound, CT scan, or MRI to assess liver size, structure, and blood flow.
- Liver Biopsy: To determine the extent and type of liver damage.
Management:
- Supportive Care: Intensive monitoring and supportive measures in a hospital setting.
- Antidotes: For specific causes, such as N-acetylcysteine for paracetamol overdose.
- Liver Transplant: In cases of fulminant liver failure when other treatments are ineffective.
- Treatment of Underlying Cause: Addressing infections, stopping offending drugs, or treating autoimmune conditions.
Chronic Liver Disease
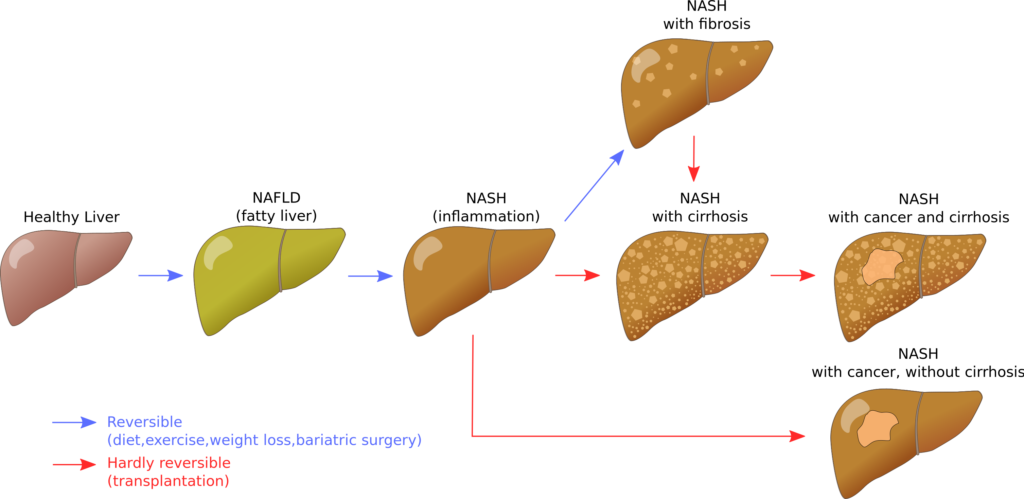
Definition: Chronic liver disease refers to liver conditions that persist for more than six months, leading to progressive damage and scarring (cirrhosis). It can eventually result in liver failure and liver cancer.
Causes:
- Chronic Viral Hepatitis: Hepatitis B and C infections.
- Alcoholic Liver Disease: Long-term excessive alcohol consumption.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Associated with obesity, diabetes, and metabolic syndrome.
- Autoimmune Hepatitis: Chronic immune-mediated liver damage.
- Genetic Disorders: Conditions like haemochromatosis (iron overload) and Wilson’s disease (copper overload).
Symptoms:
- Jaundice: Persistent yellowing of the skin and eyes.
- Ascites: Accumulation of fluid in the abdomen.
- Varices: Enlarged veins, particularly in the oesophagus and stomach, which can bleed.
- Hepatic Encephalopathy: Cognitive dysfunction ranging from confusion to coma.
- Fatigue and Weakness: General lack of energy and strength.
Diagnosis:
- Blood Tests: Liver function tests, viral hepatitis serologies, autoantibodies, and metabolic panels.
- Imaging Studies: Ultrasound, elastography (FibroScan), CT scan, or MRI to assess liver structure and fibrosis.
- Liver Biopsy: To confirm the diagnosis and stage the disease.
- Endoscopy: To detect varices and other complications.
Management:
- Lifestyle Modifications: Abstinence from alcohol, weight loss, and dietary changes.
- Medications: Antivirals for hepatitis B and C, corticosteroids for autoimmune hepatitis, and medications to manage symptoms (e.g., diuretics for ascites, lactulose for encephalopathy).
- Monitoring and Screening: Regular follow-up and screening for liver cancer.
- Liver Transplant: For patients with end-stage liver disease or liver cancer.
Process of Bacterial Translocation (A Leaky Barrier)
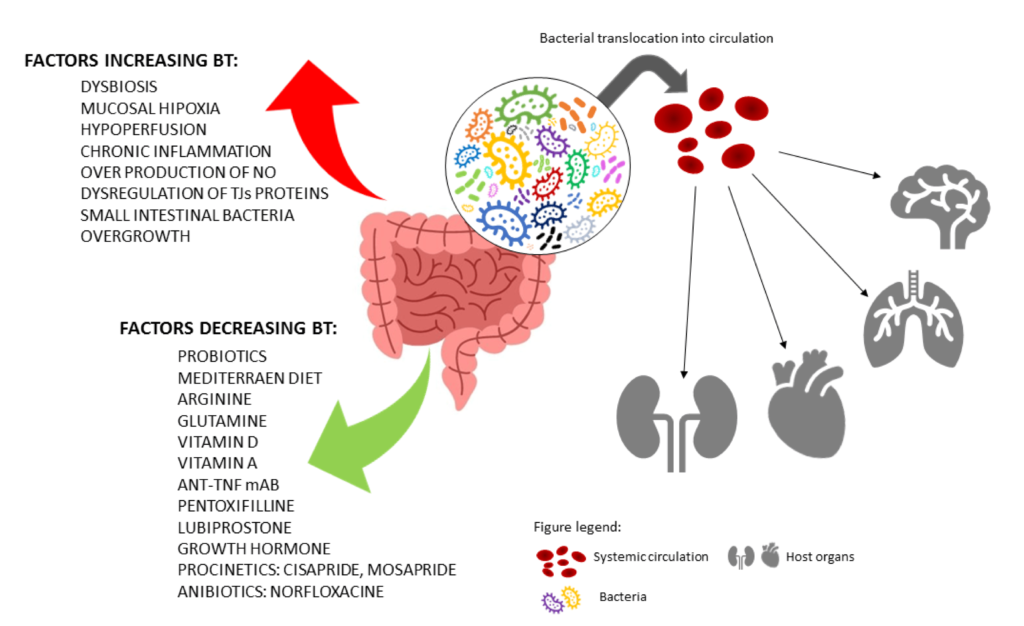
The digestive system harbors a vast number of bacteria, both beneficial and potentially harmful. Normally, a healthy gut barrier keeps these bacteria confined within the intestines. However, in liver disease, particularly chronic liver disease, this barrier can become compromised.
Definition:
Bacterial translocation refers to the migration of bacteria from the gastrointestinal (GI) tract to normally sterile tissues such as the mesenteric lymph nodes, liver, spleen, and bloodstream. This process can lead to systemic infections, chronic inflammation, and complications in patients with underlying health conditions, particularly liver disease
Mechanism:
- Intestinal Barrier Disruption:
- Conditions like cirrhosis, inflammation, or chemotherapy can damage the intestinal mucosal barrier.
- The lining of the intestine becomes more porous, allowing bacteria and their products to leak across the gut wall into the bloodstream.
- Immune System Dysfunction:
- Impaired immune response in chronic liver disease reduces the body’s ability to clear translocated bacteria.
- Changes in Gut Microbiota:
- Dysbiosis, or an imbalance in the gut microbial community, can promote bacterial overgrowth and translocation.
- An imbalance in the gut microbiome, with a decrease in beneficial bacteria and an overgrowth of harmful ones
- Increased Intestinal Permeability:
- Factors like endotoxins, alcohol, and infections can increase the permeability of the intestinal lining.
- Decreased gut motility: Slower movement of food through the intestines allows bacteria more time to proliferate and potentially breach the barrier.
Consequences:
- Systemic Infections: Bacterial translocation can lead to conditions like spontaneous bacterial peritonitis (SBP) and sepsis.
- Ascites: Fluid buildup in the abdomen.
- Sepsis: A life-threatening condition caused by the body’s overwhelming response to infection
- Hepatorenal syndrome: Kidney dysfunction due to impaired blood flow.
- Inflammation: Persistent bacterial translocation can contribute to chronic inflammation and progression of liver disease.
- Hepatic Encephalopathy: Toxins produced by translocated bacteria can exacerbate encephalopathy in patients with liver disease. Confusion and impaired brain function due to toxins affecting the brain.
Prevention and Management:
- Antibiotics: Prophylactic antibiotics like norfloxacin can reduce the risk of bacterial translocation in high-risk patients.
- Probiotics and Prebiotics: May help restore a healthy gut microbiota.
- Prokinetic Agents:
- Medications that increase gut motility can help reduce bacterial overgrowth and translocation. Examples include metoclopramide and erythromycin.
- Managing Liver Disease: Effective treatment of underlying liver conditions to maintain gut barrier function and immune response.
