Acute Respiratory Distress Syndrome (ARDS) is a severe inflammatory condition of the lungs characterised by sudden onset of widespread inflammation, leading to pulmonary oedema, decreased lung compliance, and severe hypoxaemia. It typically arises in critically ill patients and is associated with significant morbidity and mortality.
Causes
ARDS can be caused by a variety of direct and indirect lung injuries. Common causes include:
- Direct Lung Injury:
- Pneumonia
- Aspiration of gastric contents
- Inhalation of toxic substances
- Near-drowning
- Pulmonary contusion
- Indirect Lung Injury:
- Sepsis
- Severe trauma
- Pancreatitis
- Blood transfusions (transfusion-related acute lung injury – TRALI)
- Drug overdose
Signs & Symptoms
The symptoms of ARDS typically develop within a few hours to a few days after the initial injury or illness and may include:
- Severe shortness of breath
- Rapid, shallow breathing (tachypnoea)
- Cyanosis (bluish discolouration of the skin due to low oxygen levels)
- Crackles or wheezes heard in the lungs
- Hypoxaemia (low blood oxygen levels) that does not improve with oxygen therapy
- Chest pain
- Fatigue
Pathophysiology
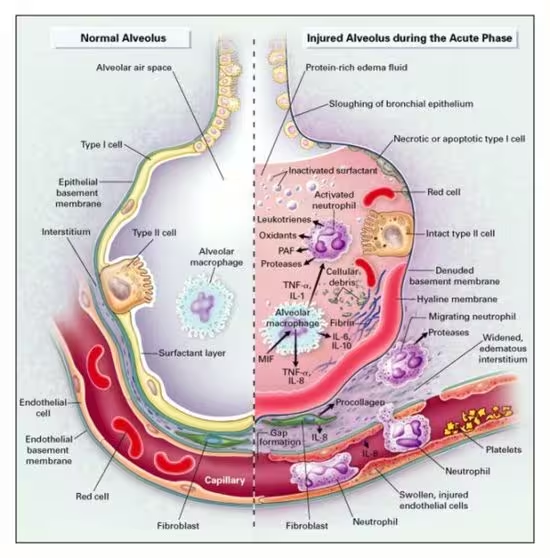
ARDS is characterised by diffuse alveolar damage and increased permeability of the alveolar-capillary barrier, leading to the following pathophysiological changes:
- Exudative Phase (1-7 days):
- Injury to the alveolar-capillary membrane causes increased permeability.
- Fluid, proteins, and inflammatory cells leak into the alveoli, leading to pulmonary oedema and reduced gas exchange.
- Formation of hyaline membranes composed of fibrin and cellular debris.
- Proliferative Phase (7-21 days):
- Type II alveolar cells proliferate to replace damaged type I cells.
- Fibroblasts begin to deposit collagen, leading to fibrosis.
- Continued inflammation and repair processes.
- Fibrotic Phase (after 3 weeks):
- Extensive fibrosis and tissue remodelling occur.
- Reduced lung compliance and increased dead space.
- Persistent hypoxaemia and risk of long-term respiratory disability.
Diagnostic Criteria
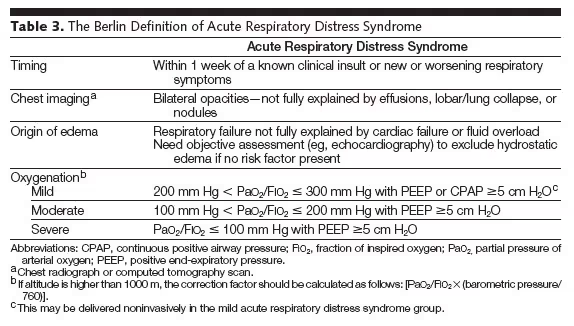
The diagnosis of ARDS is based on clinical, radiographic, and physiological criteria. The Berlin Definition is commonly used:
- Timing: Acute onset within one week of a known clinical insult or new/worsening respiratory symptoms.
- Chest Imaging: Bilateral opacities not fully explained by effusions, lobar/lung collapse, or nodules on chest X-ray or CT scan.
- Origin of Oedema: Respiratory failure not fully explained by cardiac failure or fluid overload. Objective assessment (e.g., echocardiography) to exclude hydrostatic oedema if no risk factor is present.
- Oxygenation: The severity of hypoxaemia is categorised by the PaO2/FiO2 ratio (arterial oxygen partial pressure to fractional inspired oxygen):
- Mild ARDS: 200 mmHg < PaO2/FiO2 ≤ 300 mmHg with PEEP or CPAP ≥ 5 cm H2O
- Moderate ARDS: 100 mmHg < PaO2/FiO2 ≤ 200 mmHg with PEEP ≥ 5 cm H2O
- Severe ARDS: PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 cm H2O
Management
Management of ARDS involves supportive care, addressing the underlying cause, and specific strategies to improve oxygenation and ventilation.
- Supportive Care:
- Oxygen Therapy: Administered to maintain adequate oxygen levels.
- Mechanical Ventilation: Often required to support breathing. Strategies include:
- Low tidal volume ventilation to reduce lung injury.
- Positive end-expiratory pressure (PEEP) to keep alveoli open.
- Prone positioning to improve oxygenation.
- Fluid Management:
- Conservative fluid management to minimise pulmonary oedema.
- Pharmacological Treatment:
- Use of sedatives and paralytics to facilitate mechanical ventilation.
- Antibiotics if a bacterial infection is present.
- Corticosteroids may be considered in some cases to reduce inflammation.
- Treatment of Underlying Cause:
- Addressing sepsis with appropriate antibiotics and supportive measures.
- Treating other underlying conditions such as trauma or pancreatitis.
- Adjunctive Therapies:
- Extracorporeal membrane oxygenation (ECMO) for severe, refractory hypoxaemia.
- Inhaled nitric oxide or prostacyclin to improve oxygenation in selected patients.
- Monitoring and Follow-Up:
- Regular assessment of respiratory status, oxygenation, and response to treatment.
- Long-term follow-up for survivors to address potential physical, psychological, and functional impairments.
