It occurs when the body’s immune system overreacts to a foreign substance, such as food, medication, or insect stings.
Definition:
Anaphylactic shock is a severe, life-threatening allergic reaction that occurs rapidly and can lead to death if not promptly treated. It is characterised by widespread vasodilation, increased vascular permeability, and bronchoconstriction, resulting in hypotension, respiratory distress, and multi-organ dysfunction.
Pathophysiology
Anaphylactic shock involves an immediate hypersensitivity reaction mediated by immunoglobulin E (IgE) antibodies:
1. Initial Exposure and Sensitization:
- Upon first exposure to an allergen (e.g., food, medication, insect venom), the immune system mistakenly identifies it as a harmful substance.
- This leads to the production of Immunoglobulin E (IgE) antibodies specific to that allergen.
- The IgE antibodies bind to receptors on the surface of mast cells and basophils, which are immune cells involved in allergic responses.
- The individual is now sensitized, meaning that their immune system is primed to react to the allergen if encountered again.
2. Re-Exposure and Immediate Reaction:
- Upon re-exposure to the same allergen, it binds to the IgE antibodies on the surface of mast cells and basophils.
- This cross-linking of IgE triggers the degranulation of these cells, leading to the rapid release of a large amount of pre-formed mediators such as histamine, bradykinin, and newly synthesized mediators like leukotrienes, prostaglandins, and cytokines.
- Histamine is stored in granules within mast cells and basophils. It is released when these cells are activated by allergens in the context of an allergic reaction, such as anaphylaxis. Histamine causes Vasodilation, Increased Vascular Permeability & Bronchoconstriction.
- Prostaglandins are potent vasodilators & enhance the permeability of blood vessels leading to fluid leakage from the vascular system into tissues.
- Histamine is stored in granules within mast cells and basophils. It is released when these cells are activated by allergens in the context of an allergic reaction, such as anaphylaxis. Histamine causes Vasodilation, Increased Vascular Permeability & Bronchoconstriction.
3. Mediator Release and Systemic vasodilation Effects:
- Histamine Release:
- Causes vasodilation (widening of blood vessels), leading to a significant drop in blood pressure (hypotension).
- Increases vascular permeability, causing fluid to leak from blood vessels into tissues, resulting in swelling (angioedema) and contributing further to hypotension. (Fluid shift from intravascular to interstitial compartment causing oedema)
- Induces bronchoconstriction (narrowing of the airways), leading to difficulty in breathing.
- Leukotrienes and Prostaglandins:
- These further enhance vasodilation, bronchoconstriction, and increase mucus secretion, exacerbating respiratory symptoms.
- Cytokines:
- Contribute to systemic inflammation, worsening the severity of the reaction.
- Time Frame: These symptoms can develop within minutes to an hour after exposure to the allergen.
4. Cardiovascular Collapse:
- Vasodilation and Fluid Loss:
- The profound vasodilation and fluid leakage result in a dramatic reduction in blood return to the heart (venous return), leading to decreased cardiac output.
- The heart struggles to maintain adequate blood flow, resulting in shock.
- Impaired Organ Perfusion:
- Due to the drastic drop in blood pressure, vital organs such as the brain, kidneys, and heart receive inadequate blood supply, leading to organ dysfunction.
- Compensatory Mechanisms:
- The body attempts to compensate by increasing heart rate (tachycardia), but this is often insufficient to overcome the severe hypotension and circulatory collapse.
5. Respiratory Compromise:
- Bronchoconstriction:
- The narrowing of the airways causes wheezing, shortness of breath, and can lead to respiratory failure if untreated.
- Mucus Production:
- Increased mucus secretion obstructs the airways, further complicating breathing.
- Angioedema: of lips and tongue
- Angioedema is a condition characterised by sudden, localized swelling of the deeper layers of the skin and mucous membranes.
6. Gastrointestinal and Skin Manifestations:
- Gastrointestinal Symptoms:
- The release of mediators can cause nausea, vomiting, abdominal pain, and diarrhea.
- Skin Reactions:
- Urticaria (hives) and erythema (redness) occur due to histamine’s effects on skin blood vessels.
7. Potential Fatal Outcomes:
- Without prompt treatment, the combination of cardiovascular collapse, respiratory failure, and organ dysfunction can rapidly lead to death.
Identification:
Early recognition of anaphylactic shock is crucial:
- Clinical Symptoms:
- Rapid onset following exposure to a known allergen
- Hypotension (low blood pressure)
- Tachycardia (rapid heart rate)
- Difficulty breathing (dyspnoea), wheezing, or stridor
- Swelling of the face, lips, tongue, or throat (angioedema)
- Skin reactions, such as hives (urticaria), flushing, or itching
- Gastrointestinal symptoms, such as nausea, vomiting, or diarrhoea
- Altered mental status (confusion, anxiety)
2. Physical Examination:
Symptoms of anaphylaxis include the following:
- Airway – Persistent cough, hoarse voice, difficulty swallowing, swollen tongue
- Breathing – Difficult or noisy breathing, wheeze or persistent cough
- Circulation – Dizziness, pale or floppy, suddenly sleepy, collapse/unconscious
3. Diagnostic Tests:
- Serum Tryptase: Elevated levels confirm mast cell activation.
- IgE Levels: Specific IgE testing may identify the causative allergen.
- Histamine Levels:
- Because histamine has a short half-life and is rapidly degraded, blood levels may return to normal within 30 to 60 minutes. This makes the timing of blood sample collection critical for accurate measurement
Management
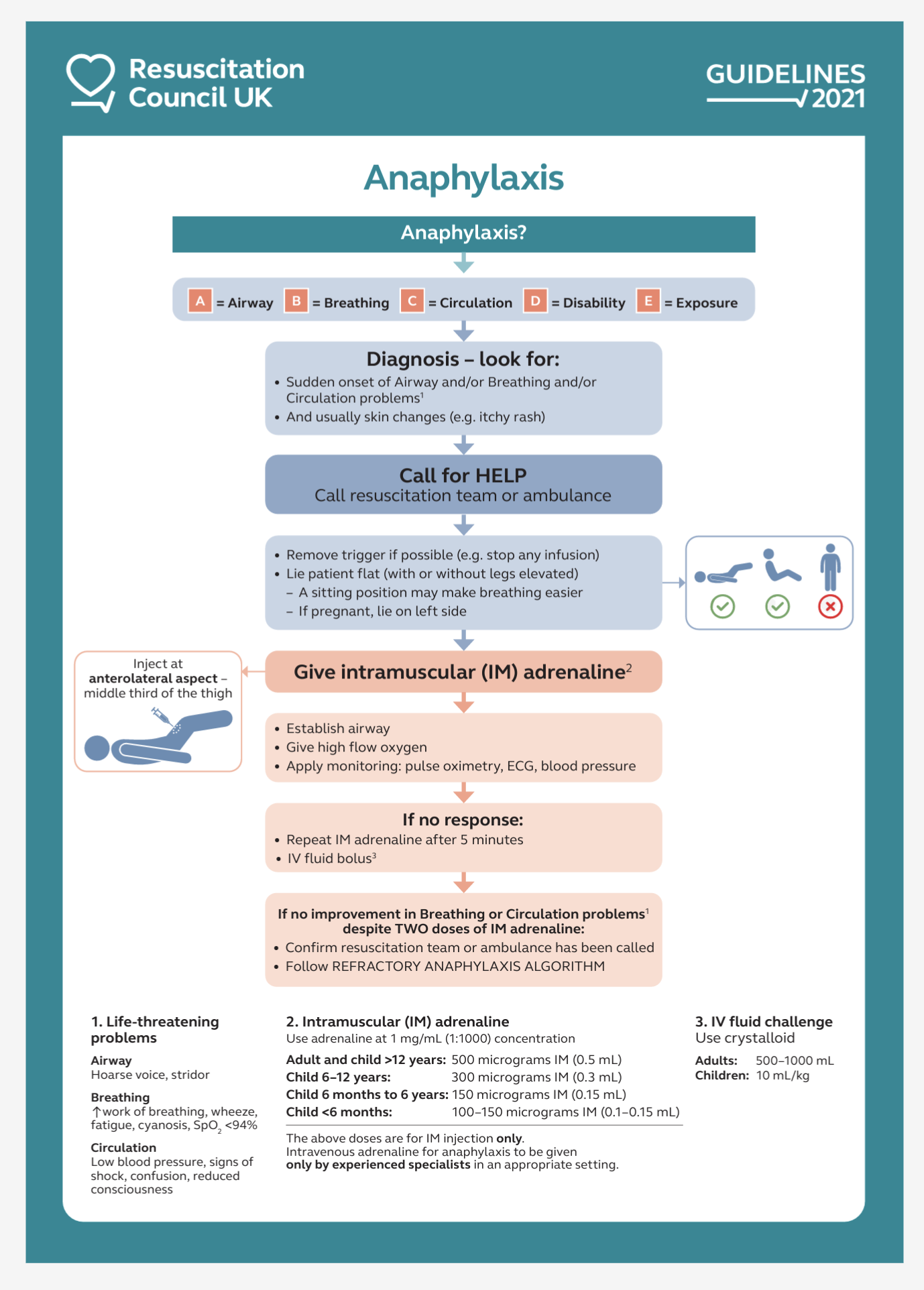
Management of anaphylactic shock focuses on rapid recognition, immediate administration of adrenaline, and supportive care:
- Initial Treatment:
- Airway Management: Ensure the airway is clear. Provide supplemental oxygen and consider advanced airway interventions if there is severe respiratory distress.
- Intravenous Access: Establish IV access for the administration of fluids and medications.
- Adrenaline: (Epinephrine): Administer intramuscular adrenaline (0.5 mg in adults or 0.01 mg/kg in children) into the mid-outer thigh immediately. Repeat every 5-15 minutes if necessary. ( Anaphylaxis UK)
- Adrenaline: As an alpha-receptor agonist, it reverses vasodilatation and reduces oedema.
- Adrenaline: As a beta-receptor, it dilates the airways, increases the force of myocardial contraction, and suppresses further histamine and leukotriene release.
- EpiPen® delivers a single dose of 0.3mg of adrenaline BP 1:1000 (0.3ml) For adult and child body weight 25kg and above – 0.3mg (Epipen UK 2024)
- EpiPen® Jr. delivers a single dose of 0.15mg adrenaline BP 1:2000 (0.3ml). For child body weight 7.5 kg- 25kg – 0.15mg (Epipen UK 2024)
2. Supportive Care:
- Fluid Resuscitation: Administer IV crystalloids (e.g., normal saline) to maintain blood pressure and perfusion.
- Antihistamines: Administer H1-antihistamines (e.g., chlorphenamine) and H2-antihistamines (e.g., ranitidine) to counteract histamine effects.
- Corticosteroids: Administer corticosteroids (e.g., hydrocortisone) to reduce the risk of biphasic reactions.
3. Monitoring and Follow-up:
- Observation: Monitor the patient closely for recurrence of symptoms. Patients should be observed for at least 4-6 hours after initial treatment.
- Education and Prevention: Educate patients on avoiding known allergens and the use of adrenaline auto-injectors. Provide an action plan for future anaphylactic episodes.
References:
