Antiarrhythmic drugs are medications used to treat and prevent abnormal heart rhythms, known as arrhythmias. These drugs work by affecting the electrical impulses in the heart to restore a normal rhythm.
Classification of Antiarrhythmic Drugs
Antiarrhythmic drugs are classified into four main classes based on the Vaughan-Williams classification system:
- Class I: Sodium Channel Blockers
- Class II: Beta-Blockers
- Class III: Potassium Channel Blockers
- Class IV: Calcium Channel Blockers
- Other Antiarrhythmic Agents
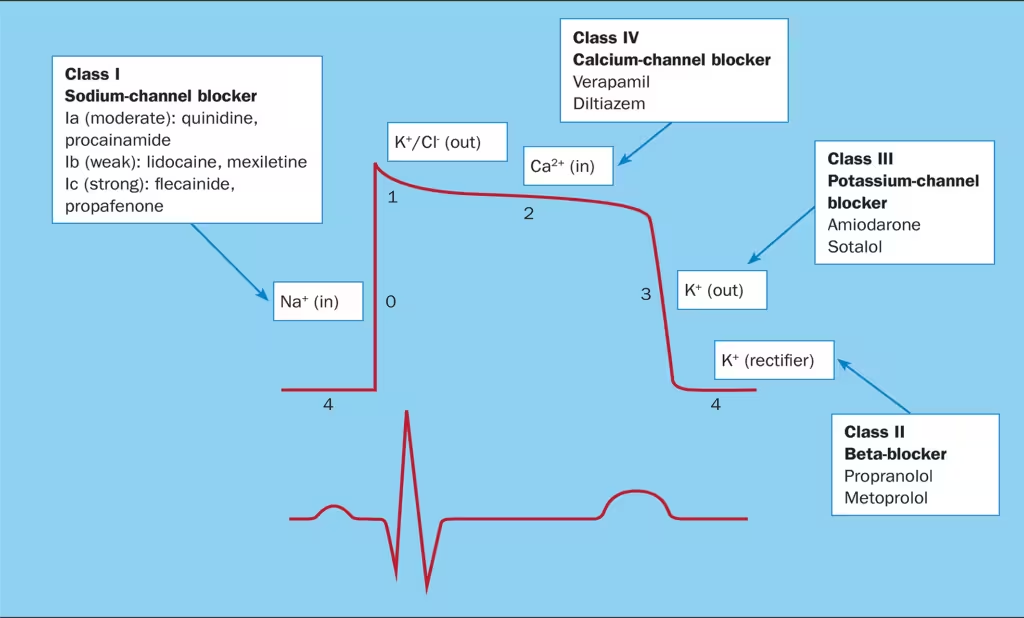
Class I: Sodium Channel Blockers
Class I antiarrhythmics are further divided into three subcategories based on their effects on the action potential duration.
- Class IA (Moderate sodium channel blockade; prolongs repolarization)
- Quinidine
- Mechanism: Blocks sodium channels and prolongs the action potential.
- Uses: Atrial fibrillation, ventricular tachycardia.
- Dose: 200-300 mg orally every 6-8 hours.
- Adverse Effects: Cinchonism (tinnitus, headache), gastrointestinal upset, torsades de pointes.
- Contraindications: Myasthenia gravis, severe heart block.
- Procainamide
- Mechanism: Similar to quinidine; also has ganglionic blocking properties.
- Uses: Atrial and ventricular arrhythmias.
- Dose: 50 mg/kg/day orally in divided doses.
- Adverse Effects: Lupus-like syndrome, agranulocytosis, torsades de pointes.
- Contraindications: Myasthenia gravis, severe heart block.
- Quinidine
- Class IB (Mild sodium channel blockade; shortens repolarization)
- Lidocaine
- Mechanism: Blocks sodium channels, and shortens action potential duration.
- Uses: Acute ventricular arrhythmias, particularly post-myocardial infarction.
- Dose: 1-1.5 mg/kg IV bolus, followed by 1-4 mg/min infusion.
- Adverse Effects: CNS toxicity (tremor, seizures), hypotension.
- Contraindications: Severe heart block without a pacemaker.
- Mexiletine
- Mechanism: Similar to lidocaine, but available orally.
- Uses: Chronic ventricular arrhythmias.
- Dose: 200-300 mg orally every 8 hours.
- Adverse Effects: Nausea, vomiting, tremor.
- Contraindications: Severe heart block without a pacemaker.
- Lidocaine
- Class IC (Marked sodium channel blockade; no effect on repolarization)
- Flecainide
- Mechanism: Blocks sodium channels with a significant slowing of conduction.
- Uses: Atrial fibrillation, supraventricular tachycardia.
- Dose: 50-200 mg orally twice daily.
- Adverse Effects: Proarrhythmia, dizziness, blurred vision.
- Contraindications: Structural heart disease, post-myocardial infarction.
- Propafenone
- Mechanism: Similar to flecainide, it also has beta-blocking effects.
- Uses: Atrial fibrillation, supraventricular tachycardia.
- Dose: 150-300 mg orally every 8 hours.
- Adverse Effects: Metallic taste, constipation, proarrhythmia.
- Contraindications: Structural heart disease, severe obstructive pulmonary disease.
- Flecainide
Class II: Beta-Blockers
Beta-blockers are often first-line antiarrhythmic therapy because of their excellent safety profile and effectiveness in treating ventricular arrhythmias
- Propranolol
- Mechanism: Non-selective beta-adrenergic blocker.
- Uses: Atrial fibrillation, supraventricular and ventricular arrhythmias.
- Propranolol is also used to prevent migraines, manage symptoms of anxiety, and treat essential tremors.
- It can be used in the management of hyperthyroidism symptoms and to reduce the risk of complications following a heart attack.
- Dose: 10-40 mg orally three to four times daily.
- Adverse Effects: Bradycardia, hypotension, bronchospasm.
- Contraindications: Asthma, severe bradycardia, heart block.
- Metoprolol
- Mechanism: Selective beta-1 adrenergic blocker.
- Uses: Atrial fibrillation, supraventricular arrhythmias.
- Dose: 50-200 mg orally twice daily.
- Adverse Effects: Bradycardia, hypotension, fatigue.
- It should not be discontinued abruptly due to the risk of rebound tachycardia or hypertension.
- Contraindications: Severe bradycardia, heart block, cardiogenic shock.
Class III: Potassium Channel Blockers
Potassium channel blockers decrease potassium efflux out of the cell and prolong the QTc interval.
- Amiodarone
- Mechanism: It works by blocking potassium channels, prolonging the cardiac action potential and repolarisation and decrease AV nodal conduction, and affecting sodium and calcium channels and beta-adrenergic receptors, which slows down the heart rate and stabilizes the heart rhythm.
- Uses: Atrial and ventricular arrhythmias.
- Dose: 200-400 mg orally daily,
- IV for acute use.
- Loading dose: 300 mg IV with 5% Dextrose 100 ml over 1 hour
- Maintenance dose: 900 mg IV with 5% Dextrose 50 ml infusion over 23 hours on day 1.
- A repeated dose of 900 mg by infusion over 24 hours can be given on subsequent days if required
- Adverse Effects: Pulmonary fibrosis, thyroid dysfunction, liver toxicity.
- Contraindications: Severe sinus node dysfunction, 2nd or 3rd degree heart block.
- Sotalol
- Mechanism: Non-selective beta-blocker with potassium channel blocking properties.
- Uses: Atrial and ventricular arrhythmias.
- Dose: 80-160 mg orally twice daily.
- Adverse Effects: Torsades de pointes, bradycardia.
- Contraindications: Severe renal impairment, asthma, bradycardia.
Class IV: Calcium Channel Blockers
Non-dihydropyridine calcium channel blockers (diltiazem, verapamil) decrease conduction velocity and slow conduction through the AV node
- Verapamil
- Mechanism: Blocks L-type calcium channels, reducing heart rate and contractility.
- Uses: Supraventricular tachycardia, rate control in atrial fibrillation.
- Dose: 120-360 mg orally daily in divided doses.
- Adverse Effects: Constipation, bradycardia, hypotension.
- Contraindications: Severe left ventricular dysfunction, hypotension, heart block.
- Diltiazem
- Mechanism: Similar to verapamil, with less negative inotropic effect.
- Uses: Supraventricular tachycardia, rate control in atrial fibrillation.
- Dose: 120-360 mg orally daily in divided doses.
- Adverse Effects: Edema, bradycardia, hypotension.
- Contraindications: Severe left ventricular dysfunction, hypotension, heart block.
Other Antiarrhythmic Agents
- Adenosine
- Mechanism: Activates adenosine receptors, causing transient heart block in the AV node.
- Uses: Acute termination of supraventricular tachycardia.
- Dose: 6-12 mg IV push.
- Adverse Effects: Flushing, chest pain, bronchospasm.
- Contraindications: Asthma, second or third-degree heart block.
- Digoxin-Digoxin is generally not the first choice for controlling ventricular rate in atrial fibrillation (AF). However, using a combination of digoxin with a beta-blocker or a non-dihydropyridine calcium channel blocker can be a suitable option for rate control in patients with AF and heart failure
- Mechanism: Inhibits Na+/K+ ATPase, increasing vagal tone and slowing AV conduction.
- Uses: Atrial fibrillation, heart failure.
- Dose: 0.125-0.25 mg orally daily.
- Adverse Effects: Nausea, vomiting, visual disturbances, arrhythmias.
- Contraindications: Ventricular fibrillation, digoxin hypersensitivity.
Clinical Use and Guidelines
In the UK, the use of antiarrhythmic drugs is guided by clinical guidelines from authoritative bodies such as the National Institute for Health and Care Excellence (NICE).
- Atrial Fibrillation:
- Rate Control: Beta-blockers (e.g., metoprolol), calcium channel blockers (e.g., diltiazem), and digoxin.
- Rhythm Control: Amiodarone, flecainide, propafenone.
- Supraventricular Tachycardia:
- Acute Management: Adenosine, verapamil.
- Chronic Management: Beta-blockers, calcium channel blockers.
- Ventricular Arrhythmias:
- Acute Management: Amiodarone, lidocaine.
- Chronic Management: Beta-blockers, amiodarone, sotalol.
Monitoring and Adverse Effects
Regular monitoring is crucial to ensure the safety and efficacy of antiarrhythmic drugs:
- Electrocardiogram (ECG): To monitor heart rhythm and detect proarrhythmic effects.
- Serum Levels: For drugs like digoxin to ensure therapeutic levels.
- Renal and Liver Function: To adjust dosages and prevent toxicity, especially for drugs like amiodarone and sotalol.
