Antihypertensive drugs are medications used to manage high blood pressure (hypertension). They work through various mechanisms to lower blood pressure, thus reducing the risk of cardiovascular events such as heart attack and stroke. Here’s a detailed overview of the main classes of antihypertensive drugs, including their mechanisms of action, clinical uses, dosages, adverse effects, and contraindications, aligned with UK standards and clinical guidelines.
Major Classes of Antihypertensive Drugs
- Angiotensin-converting enzyme (ACE) Inhibitors
- Angiotensin II Receptor Blockers (ARBs)
- Calcium Channel Blockers (CCBs)
- Diuretics
- Beta-Blockers
- Alpha-Blockers
- Central Alpha-2 Agonists
- Direct Vasodilators
1. ACE Inhibitors
Examples: Enalapril, Lisinopril, Ramipril
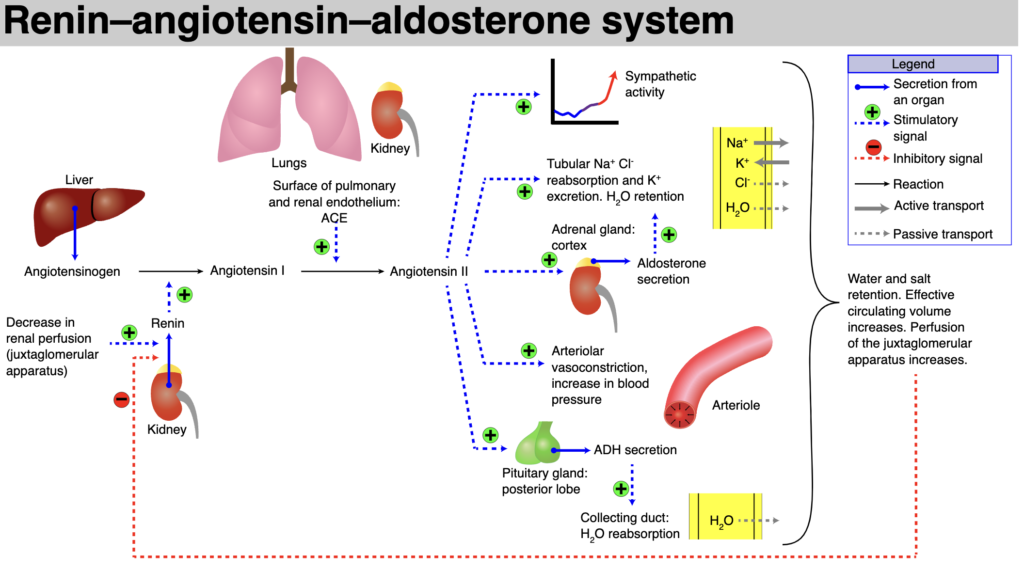
- Mechanism: Inhibit the angiotensin-converting enzyme, reducing the conversion of angiotensin I to angiotensin II, a potent vasoconstrictor. This leads to vasodilation and decreased blood pressure.
- Uses: Hypertension, heart failure, post-myocardial infarction, diabetic nephropathy.
- Dosage:
- Enalapril: 5-20 mg orally daily.
- Lisinopril: 10-40 mg orally daily.
- Ramipril: 2.5-10 mg orally daily.
- Adverse Effects: Cough, hyperkalemia, hypotension, renal impairment, angioedema.
- Contraindications: Pregnancy, history of angioedema, bilateral renal artery stenosis.
2. ARBs
Examples: Losartan, Valsartan, Candesartan
- Mechanism: Block the angiotensin II receptors, preventing angiotensin II from exerting its vasoconstrictor effects, leading to vasodilation and reduced blood pressure.
- Uses: Hypertension, heart failure, diabetic nephropathy, post-myocardial infarction.
- Dosage:
- Losartan: 50-100 mg orally daily.
- Valsartan: 80-320 mg orally daily.
- Candesartan: 8-32 mg orally daily.
- Adverse Effects: Hyperkalemia, hypotension, renal impairment, dizziness.
- Contraindications: Pregnancy, severe renal impairment.
3. Calcium Channel Blockers (CCBs)
Examples: Amlodipine, Diltiazem, Verapamil
- Mechanism: Inhibit the influx of calcium ions into vascular smooth muscle and cardiac muscle, leading to vasodilation and decreased heart contractility.
- Uses: Hypertension, angina, certain arrhythmias.
- Dosage:
- Amlodipine: 5-10 mg orally daily.
- Diltiazem: 120-360 mg orally daily in divided doses.
- Verapamil: 80-120 mg orally three times daily.
- Adverse Effects: Peripheral edema, bradycardia, constipation, dizziness.
- Contraindications: Severe hypotension, and severe left ventricular dysfunction.
4. Diuretics
Examples: Hydrochlorothiazide, Furosemide, Spironolactone
- Mechanism: Increase the excretion of sodium and water from the kidneys, reducing blood volume and pressure.
- Types and Uses:
- Thiazide Diuretics (e.g., Hydrochlorothiazide): First-line for hypertension.
- Loop Diuretics (e.g., Furosemide): Used in heart failure and edema.
- Potassium-Sparing Diuretics (e.g., Spironolactone): Used in combination with other diuretics to prevent hypokalemia.
- Dosage:
- Hydrochlorothiazide: 12.5-50 mg orally daily.
- Furosemide: 20-80 mg orally daily.
- Spironolactone: 25-100 mg orally daily.
- Adverse Effects: Electrolyte imbalance, dehydration, hypotension, hyperkalemia (for potassium-sparing diuretics).
- Contraindications: Severe renal impairment, anuria, hyperkalemia (for potassium-sparing diuretics).
5. Beta-Blockers
Examples: Atenolol, Metoprolol, Carvedilol
- Mechanism: Block beta-adrenergic receptors, reducing heart rate and cardiac output, which lowers blood pressure.
- Uses: Hypertension, angina, heart failure, post-myocardial infarction.
- Dosage:
- Atenolol: 25-100 mg orally daily.
- Metoprolol: 50-200 mg orally daily.
- Carvedilol: 3.125-25 mg orally twice daily.
- Adverse Effects: Bradycardia, hypotension, fatigue, bronchospasm.
- Contraindications: Asthma, severe bradycardia, heart block.
6. Alpha-Blockers
Examples: Doxazosin, Prazosin
- Mechanism: Block alpha-adrenergic receptors, leading to vasodilation and decreased blood pressure.
- Uses: Hypertension, benign prostatic hyperplasia.
- Dosage:
- Doxazosin: 1-16 mg orally daily.
- Prazosin: 1-5 mg orally two to three times daily.
- Adverse Effects: Orthostatic hypotension, dizziness, headache.
- Contraindications: History of orthostatic hypotension, and severe liver impairment.
7. Central Alpha-2 Agonists
Examples: Clonidine, Methyldopa
- Mechanism: Stimulate alpha-2 adrenergic receptors in the brain, reducing sympathetic outflow and lowering blood pressure.
- Uses: Hypertension (particularly in pregnancy for methyldopa).
- Dosage:
- Clonidine: 0.1-0.3 mg orally twice daily.
- Methyldopa: 250-500 mg orally two to three times daily.
- Adverse Effects: Sedation, dry mouth, rebound hypertension (on abrupt withdrawal).
- Contraindications: Active liver disease (for methyldopa).
8. Direct Vasodilators
Examples: Hydralazine, Minoxidil
- Mechanism: Directly relax vascular smooth muscle, causing vasodilation and lowering blood pressure.
- Uses: Hypertension, hypertensive emergencies (for hydralazine).
- Dosage:
- Hydralazine: 10-50 mg orally four times daily.
- Minoxidil: 5-40 mg orally daily.
- Adverse Effects: Reflex tachycardia, fluid retention, lupus-like syndrome (for hydralazine).
- Contraindications: Severe coronary artery disease, rheumatic heart disease (for hydralazine).
Clinical Use and Guidelines
In the UK, the use of antihypertensive drugs is guided by clinical guidelines from authoritative bodies such as the National Institute for Health and Care Excellence (NICE).
- Hypertension:
- First-line treatment typically includes ACE inhibitors, ARBs, CCBs, or thiazide diuretics.
- Combination therapy is often required for adequate blood pressure control.
- Heart Failure:
- ACE inhibitors or ARBs, beta-blockers, and diuretics are commonly used.
- Spironolactone or eplerenone may be added for severe heart failure.
- Post-Myocardial Infarction:
- Beta-blockers and ACE inhibitors are recommended to reduce mortality.
- Chronic Kidney Disease:
- ACE inhibitors or ARBs are preferred due to their protective effects on the kidneys.
Monitoring and Adverse Effects
Regular monitoring is essential to ensure the safety and efficacy of antihypertensive drugs:
- Blood Pressure: To assess the effectiveness of treatment.
- Electrolytes: Particularly with diuretics and ACE inhibitors/ARBs to detect imbalances.
- Renal Function: Periodically check serum creatinine and eGFR, especially with ACE inhibitors and ARBs.
- Liver Function: Monitoring may be required for drugs like methyldopa.
