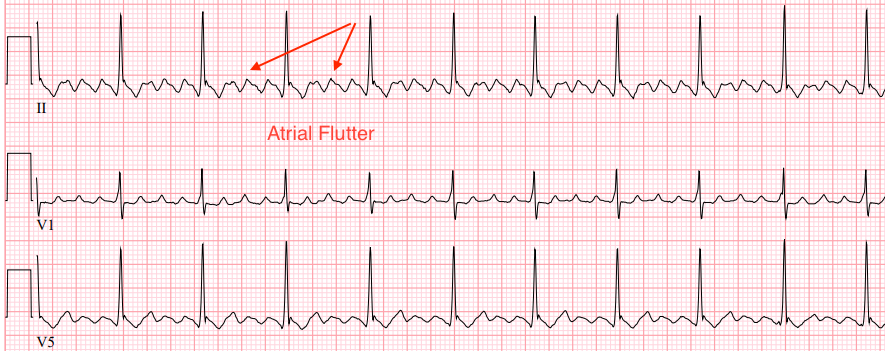
Atrial flutter is a type of supra-ventricular tachycardia characterised by a rapid, regular heartbeat originating from the atria. This condition is often associated with a “sawtooth” pattern on an electrocardiogram (ECG), indicating the rapid and organised nature of atrial electrical activity. Understanding the pathophysiology, causes, symptoms, diagnostic criteria, and treatment options for atrial flutter is crucial for effective management and care.
Pathophysiology
Atrial flutter occurs due to a reentrant circuit within the atria, typically in the right atrium. This reentrant circuit causes the atria to contract at a very high rate, often between 240 to 340 beats per minute. However, not all these atrial impulses are conducted to the ventricles due to the limiting function (Refractory property) of the atrioventricular (AV) node, leading to a ventricular rate that is often lower than the atrial rate.
Types of Atrial Flutter
- Typical Atrial Flutter:
- Counterclockwise Flutter: The most common type, where the reentrant circuit circles around the tricuspid valve in a counterclockwise direction when viewed from above. This produces the characteristic “sawtooth” pattern of flutter waves, particularly visible in the inferior leads (II, III, and aVF) on an ECG.
- Clockwise Flutter: A less common variation of typical flutter, where the reentrant circuit moves in a clockwise direction around the tricuspid valve.
2. Atypical Atrial Flutter:
- Right Atrial Atypical Flutter: This involves reentrant circuits in other locations within the right atrium that are not typical circuits around the tricuspid valve.
- Left Atrial Flutter: This involves reentrant circuits in the left atrium. Atypical flutter can occur post-cardiac surgery, post-catheter ablation for atrial fibrillation, or due to other structural heart diseases.
Causes
Atrial flutter can be triggered by various factors and conditions that affect the heart’s electrical system:
- Structural Heart Disease: Conditions such as ischaemic heart disease, cardiomyopathy, and heart valve disorders can predispose individuals to atrial flutter.
- Post-Surgical State: Patients who have undergone cardiac surgery, particularly involving the atria, are at increased risk.
- Hypertension: High blood pressure can lead to structural changes in the heart, contributing to atrial flutter.
- Pulmonary Conditions: Chronic obstructive pulmonary disease (COPD) and pulmonary embolism are known triggers.
- Alcohol and Drugs: Excessive alcohol consumption and the use of stimulants such as caffeine or illicit drugs can provoke atrial flutter.
Symptoms
The symptoms of atrial flutter are often related to the rapid heart rate and reduced cardiac efficiency:
- Palpitations: A sensation of rapid, fluttering, or pounding heartbeats.
- Shortness of Breath: Difficulty breathing due to inefficient blood circulation.
- Fatigue: Generalised tiredness and weakness.
- Dizziness or Lightheadedness: Due to reduced blood flow to the brain.
- Chest Pain: Discomfort or pain in the chest, which may indicate myocardial ischaemia.
- Syncope: In severe cases, the decreased cardiac output can lead to fainting spells.
Diagnostic Criteria
Atrial flutter is diagnosed primarily through an electrocardiogram (ECG):
- ECG Patterns: The hallmark “sawtooth” flutter waves are best seen in leads II, III, and aVF, indicating rapid and regular atrial activity.
- Ventricular Rate: The ventricular rate may be regular or irregular depending on the AV conduction ratio but is typically around 150 beats per minute with a 2:1 block.
- Holter Monitor: Continuous ECG monitoring over 24-48 hours can capture intermittent atrial flutter episodes.
- Echocardiogram: An ultrasound of the heart may be performed to assess structural heart disease and atrial size.
Guidelines for the Management of Atrial Flutter in the ICU in the UK
Management of atrial flutter in the ICU in the UK involves initial stabilization, rate and rhythm control, anticoagulation, and consideration of long-term strategies such as catheter ablation. Guidelines from NICE, ESC, and other authoritative bodies provide detailed recommendations to ensure effective and safe patient care
1. Initial Assessment and Monitoring
- Vital Signs Monitoring: Continuous monitoring of ECG, blood pressure, oxygen saturation, and respiratory rate.
- Haemodynamic Stability: Assess for signs of haemodynamic instability, such as hypotension, shock, or heart failure.
- Symptoms Evaluation: Document symptoms including palpitations, chest pain, dyspnea, and syncope.
2. Immediate Management for Hemodynamically Unstable Patients
For patients with severe symptoms or hemodynamic instability:
- Electrical Cardioversion:
- Immediate synchronised electrical cardioversion is recommended.
- Initial energy settings: Start with 50-100 Joules and increase if necessary.
3. Management for Haemodynamically Stable Patients
For patients without severe symptoms or instability:
- Rate Control:
- Beta-Blockers (e.g., Metoprolol): To control ventricular rate.
- Calcium Channel Blockers (e.g., Diltiazem, Verapamil): As an alternative to beta-blockers.
- Digoxin: May be considered in patients with heart failure or contraindications to beta-blockers and calcium channel blockers.
- Rhythm Control:
- Pharmacological Cardioversion: Antiarrhythmic drugs such as amiodarone, flecainide (if no structural heart disease), or sotalol.
- Electrical Cardioversion: If pharmacological cardioversion is unsuccessful or not preferred.
- Anticoagulation:
- Thromboembolic Risk Assessment: Use the CHA2DS2-VASc score to assess the risk of stroke.
- Anticoagulation Therapy: Initiate anticoagulation based on the risk assessment. Options include warfarin or direct oral anticoagulants (DOACs) such as apixaban, rivaroxaban, or dabigatran.
- Peri-Cardioversion Anticoagulation: Ensure at least 3 weeks of therapeutic anticoagulation before elective cardioversion or perform a transesophageal echocardiogram (TEE) to exclude atrial thrombus.
4. Long-Term Management and Follow-Up
- Catheter Ablation:
- Consider catheter ablation for patients with recurrent atrial flutter, particularly if they are symptomatic despite medical therapy.
- Radiofrequency ablation targeting the cavotricuspid isthmus is the standard procedure for typical atrial flutter.
- Medication Review:
- Regularly review and adjust medications based on efficacy and side effects.
- Address any contributing factors such as hypertension, coronary artery disease, and other comorbidities.
- Lifestyle Modifications:
- Advise on lifestyle changes including smoking cessation, reducing alcohol intake, maintaining a healthy weight, and engaging in regular physical activity.
- Patient Education:
- Educate patients about the signs and symptoms of atrial flutter, the importance of medication adherence, and when to seek medical help.
References and Further Reading
- NICE Guidelines:
- NICE Clinical Guideline [CG180]: “Atrial fibrillation: management.” This guideline includes recommendations for the management of atrial flutter as well.
- Website: NICE
Summary
Atrial flutter is a rapid, regular heart rhythm disorder resulting from a reentrant circuit within the atria. It is characterised by a “sawtooth” pattern on ECG and can lead to symptoms such as palpitations, shortness of breath, and chest pain. There are two main types of atrial flutter: typical and atypical, with typical flutter being the more common type involving a reentrant circuit around the tricuspid valve. Diagnosing atrial flutter involves ECG and sometimes echocardiogram or Holter monitoring. Treatment aims to control the heart rate, restore normal rhythm, and prevent recurrence, often involving medications, cardioversion, catheter ablation, and anticoagulation to mitigate the risk of stroke. Understanding the pathophysiology, causes, and management of atrial flutter is essential for effective patient care.
