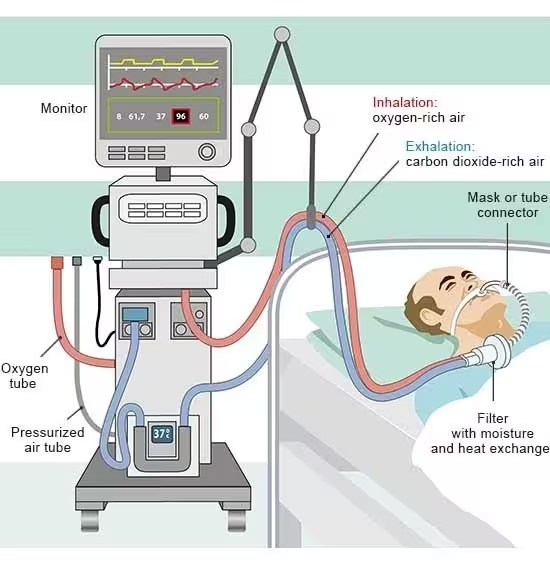
Invasive ventilation therapies are medical procedures used to assist or replace spontaneous breathing in patients who are unable to breathe adequately on their own. These therapies are commonly used in critical care settings, such as intensive care units (ICUs), during surgery, or in emergency situations.
Types of Invasive Ventilation
- Mechanical Ventilation: The primary form of invasive ventilation where a machine (ventilator) helps patients breathe.
- Endotracheal Intubation: A tube is inserted through the mouth or nose into the trachea.
- Tracheostomy: A surgical procedure to create an opening in the neck to place a tube directly into the trachea.
Indications
- Acute Respiratory Distress Syndrome (ARDS)
- Description: ARDS is a severe inflammatory condition of the lungs, resulting in widespread inflammation, increased pulmonary vascular permeability, and decreased lung compliance. It leads to significant hypoxemia (low blood oxygen levels) despite the administration of high concentrations of oxygen.
- Indication for Ventilation: Invasive ventilation is used to provide adequate oxygenation and ventilation while minimising lung injury through protective strategies such as low tidal volumes and appropriate PEEP (Positive End-Expiratory Pressure).
2) Severe Pneumonia
- Description: Pneumonia involves infection and inflammation of the alveoli in the lungs, leading to fluid accumulation and impaired gas exchange.
- Indication for Ventilation: Invasive ventilation is indicated when pneumonia leads to respiratory failure or when non-invasive methods fail to maintain adequate oxygenation and ventilation.
3) Chronic Obstructive Pulmonary Disease (COPD) Exacerbation
- Description: COPD exacerbations cause acute worsening of respiratory symptoms, including increased breathlessness, sputum production, and hypoxemia.
- Indication for Ventilation: When non-invasive ventilation fails, the patient is unable to protect their airway, or there is severe respiratory acidosis (pH < 7.25), invasive ventilation is necessary.
4) Neuromuscular Diseases
- Description: Diseases such as amyotrophic lateral sclerosis (ALS), myasthenia gravis, or spinal cord injuries can weaken the respiratory muscles, compromising their ability to maintain adequate ventilation.
- Indication for Ventilation: Invasive ventilation is required when respiratory muscles are too weak to sustain adequate ventilation, leading to respiratory failure.
5) Cardiac Arrest and Resuscitation
- Description: During and after resuscitation from cardiac arrest, patients often have impaired consciousness and respiratory efforts, necessitating controlled ventilation and oxygenation.
- Indication for Ventilation: Invasive ventilation supports stable and adequate oxygenation and facilitates other necessary treatments in post-resuscitation care.
6) Severe Trauma
- Description: Trauma to the chest or head can result in compromised respiratory function due to direct injury to the lungs and airways or due to neurological impairment.
- Indication for Ventilation: Invasive ventilation is used to stabilise breathing and protect the airway in patients with significant trauma.
7) Postoperative Care
- Description: Major surgeries, especially those involving the thoracic or abdominal cavities, can impair spontaneous breathing due to pain, sedation, or the effects of anaesthesia.
- Indication for Ventilation: Postoperative patients may require invasive ventilation to support breathing until they can maintain adequate respiratory function independently.
8) Drug Overdose
- Description: Overdose of certain medications, particularly central nervous system depressants such as opioids or sedatives, can lead to respiratory depression or arrest.
- Indication for Ventilation: Invasive ventilation is necessary to maintain adequate oxygenation and ventilation while the effects of the drug overdose are managed and reversed.
9) Accidental Removal of Breathing Tube
- Description: Accidental extubation can lead to acute respiratory failure, especially if the patient is not yet ready to breathe on their own.
- Indication for Ventilation: Reintubation and invasive ventilation are required to ensure the patient receives adequate respiratory support.
10) Improper Reversal of Anaesthetic Drugs
- Description: Inadequate reversal of anaesthetic agents post-surgery can result in residual sedation and muscle relaxation, leading to insufficient spontaneous breathing.
- Indication for Ventilation: Invasive ventilation is necessary to support the patient’s breathing until the effects of the anaesthetic drugs have fully worn off and the patient regains adequate respiratory function.
Ventilator Settings and Parameters
- Tidal Volume (Vt)
- Description: The volume of air delivered to the lungs with each breath.
- Typical Setting: 6-8 mL/kg of ideal body weight.
- Considerations: In ARDS, lower tidal volumes (4-6 mL/kg) are often used to prevent lung injury.
- Respiratory Rate (RR)
- Description: The number of breaths delivered by the ventilator per minute.
- Typical Setting: 12-20 breaths per minute, adjusted based on the patient’s needs and underlying condition.
- Fraction of Inspired Oxygen (FiO2)
- Description: The percentage of oxygen in the air mixture delivered to the patient.
- Typical Setting: 21-100%, with the goal of maintaining adequate oxygenation (PaO2 > 60 mmHg or SpO2 > 90%).
- Positive End-Expiratory Pressure (PEEP)
- Description: The pressure in the lungs (above atmospheric pressure) that remains at the end of expiration.
- Typical Setting: 5-10 cmH2O, higher in cases of ARDS to prevent alveolar collapse.
- Peak Inspiratory Pressure (PIP)
- Description: The maximum pressure applied during inhalation.
- Typical Setting: Should be kept below 30 cmH2O to avoid barotrauma.
- Inspiratory to Expiratory (I/E) Ratio
- Description: The ratio of the duration of inhalation to exhalation.
- Typical Setting: Usually set at 1:2 or 1:3 to mimic natural breathing; in ARDS, a ratio of 1:1 or inverse ratio ventilation may be used.
- Ramp Settings
- Description: Controls the time it takes for the ventilator to reach the set inspiratory pressure.
- Typical Setting: Adjusted based on patient comfort and to ensure adequate ventilation without causing barotrauma. A gradual ramp-up may be used to prevent sudden pressure increases.
- Trigger Sensitivity
- Description: Determines how much effort the patient needs to initiate a breath.
- Typical Setting: Set to ensure the patient can easily trigger a breath without auto-triggering.
- Pressure Trigger– Sensitivity is typically set between -1 to -2 cmH2O.
- Flow Trigger– Sensitivity is usually set between 1 to 3 L/min.
- Pressure Support (PS)
- Description: Additional pressure provided during spontaneous breaths to reduce the work of breathing.
- Typical Setting: Usually set between 5-20 cmH2O, adjusted to achieve adequate tidal volume and reduce respiratory muscle workload.
- Flow Rate
- Description: The speed at which the ventilator delivers the breath.
- Typical Setting: 40-60 L/min; adjusted based on patient comfort and ventilatory demand.
- Inspiratory Time (Ti)
- Description: The duration of the inspiratory phase.
- Typical Setting: Typically set at 0.8-1.2 seconds, adjusted based on the I/E ratio and patient’s needs.
Ventilatory Modes and Their Indications
Volume-Controlled Ventilation (VCV)
- Description: Delivers a preset tidal volume with each breath. The pressure varies depending on lung compliance and airway resistance.
- Indication: Used for patients with stable respiratory mechanics, post-surgery, and ARDS.
Pressure-Controlled Ventilation (PCV)
- Description: Delivers air until a preset pressure is reached. Tidal volume varies.
- Indication: Suitable for patients with low lung compliance, such as those with ARDS, and for preventing barotrauma.
Assist-Control Ventilation (A/C)
- Description: Delivers a preset volume or pressure in response to the patient’s efforts. Provides full support if the patient fails to initiate a breath.
- Indication: Used for critically ill patients, post-surgical care, and severe respiratory failure.
Synchronised Intermittent Mandatory Ventilation (SIMV)
- Description: Delivers a preset number of mandatory breaths synchronised with the patient’s efforts, allowing spontaneous breaths in between.
- Indication: Commonly used during weaning from ventilation and for partial respiratory support.
Pressure Support Ventilation (PSV)
- Description: Augments spontaneous breaths with a preset pressure. Reduces the work of breathing.
- Indication: Often used during the final stages of weaning and for patients with chronic respiratory failure.
Continuous Positive Airway Pressure (CPAP)
- Description: Provides constant positive pressure throughout the respiratory cycle.
- Indication: Used for conditions like sleep apnoea, cardiogenic pulmonary oedema, and as a trial for weaning from ventilation.
Bi-Level Positive Airway Pressure (BiPAP)
- Description: Provides two levels of pressure – higher during inhalation (IPAP) and lower during exhalation (EPAP).
- Indication: Suitable for COPD exacerbations, acute respiratory failure, and heart failure.
Monitoring and Maintenance of Invasive Ventilation
Monitoring and maintenance of invasive ventilation are critical to ensure patient safety, optimise ventilatory support, and minimise complications. Here are the key aspects involved:
Monitoring
- Ventilator Parameters
- Tidal Volume (Vt): Ensure the set and delivered tidal volumes are appropriate for the patient’s condition.
- Respiratory Rate (RR): Monitor the set and actual respiratory rate.
- FiO2: Adjust the fraction of inspired oxygen to maintain adequate oxygenation.
- PEEP: Check and adjust Positive End-Expiratory Pressure to prevent alveolar collapse.
- Peak Inspiratory Pressure (PIP): Monitor to avoid barotrauma.
- Patient Parameters
- Oxygenation: Continuous monitoring of SpO2 (pulse oximetry) and periodic arterial blood gases (ABGs) to assess PaO2 and SaO2.
- Ventilation: Monitoring end-tidal CO2 (EtCO2) and periodic ABGs to assess PaCO2.
- Lung Compliance and Resistance: Evaluate dynamic and static compliance and airway resistance to assess lung mechanics.
- Hemodynamics: Monitor blood pressure, heart rate, and other vital signs to ensure cardiovascular stability.
- Alarm Settings
- High and Low Pressure Alarms: Set to alert if airway pressures exceed safe limits or drop unexpectedly.
- High and Low Tidal Volume Alarms: Set to detect deviations from the expected tidal volume.
- Apnea Alarm: Ensures the ventilator alerts if the patient fails to initiate a breath within a set time.
Maintenance
- Regular Assessment
- Ventilator Checks: Perform regular checks to ensure the ventilator is functioning correctly and settings are appropriate.
- Circuit Inspections: Inspect the ventilator circuit for disconnections, leaks, or obstructions.
- Humidification: Ensure the humidifier is functioning properly to prevent mucosal drying and secretions buildup.
- Suctioning
- Indication: Perform endotracheal suctioning as needed to clear secretions and maintain airway patency.
- Technique: Use sterile technique to minimise the risk of infection.
- Positioning
- Patient Positioning: Reposition the patient regularly to prevent pressure ulcers and improve ventilation/perfusion matching.
- Head of Bed Elevation: Elevate the head of the bed to reduce the risk of ventilator-associated pneumonia (VAP).
- Sedation and Analgesia
- Sedation Protocols: Use sedation and analgesia to ensure patient comfort and compliance with mechanical ventilation. Regularly assess and adjust sedation levels.
- Sedation Holidays: Conduct daily sedation interruptions to assess readiness for weaning.
- Preventing Complications
- Ventilator-Associated Pneumonia (VAP) Prevention: Implement VAP prevention strategies, such as oral care with chlorhexidine, subglottic secretion drainage, and maintaining proper cuff pressure.
- DVT Prophylaxis: Use prophylactic measures to prevent deep vein thrombosis.
- Stress Ulcer Prophylaxis: Administer medications to prevent stress-related mucosal damage.
Weaning and Extubation
- Weaning Readiness
- Assessment: Regularly assess the patient’s readiness to wean from mechanical ventilation using criteria such as improved lung mechanics, adequate oxygenation, and stable hemodynamics.
- Spontaneous Breathing Trials (SBTs): Conduct trials to evaluate the patient’s ability to breathe without ventilatory support.
- Extubation
- Criteria: Ensure the patient meets extubation criteria, including adequate mental status, minimal secretions, and strong cough reflex.
- Post-Extubation Care: Monitor the patient closely post-extubation for signs of respiratory distress and provide appropriate support.
Risks and Complications of Invasive Ventilation
Invasive ventilation, while life-saving, carries several risks and potential complications. Understanding these helps in preventing, recognising, and managing them effectively.
- Ventilator-Associated Pneumonia (VAP)
- Description: Pneumonia that develops 48 hours or more after endotracheal intubation.
- Causes: Aspiration of secretions, colonisation of the respiratory tract, and contaminated equipment.
- Prevention: Elevating the head of the bed, regular oral care, subglottic suctioning, and maintaining proper cuff pressure.
- Barotrauma
- Description: Injury to the lung tissues caused by excessive airway pressure.
- Causes: High tidal volumes or peak inspiratory pressures, PEEP.
- Prevention: Using lung-protective ventilation strategies, including lower tidal volumes and appropriate PEEP levels.
- Volutrauma
- Description: Lung injury caused by overdistension of alveoli due to excessive volume.
- Causes: High tidal volumes.
- Prevention: Utilising low tidal volume strategies and careful monitoring of ventilatory settings.
- Atelectasis
- Description: Collapse of part or all of a lung, leading to reduced gas exchange.
- Causes: Blockage of airways, inadequate ventilation, mucus plugs.
- Prevention: Regular suctioning, ensuring adequate humidification, and adjusting ventilator settings to promote lung expansion.
- Pneumothorax
- Description: Accumulation of air in the pleural space, causing lung collapse.
- Causes: Rupture of alveoli due to high pressures or volumes.
- Prevention: Monitoring and limiting airway pressures and volumes.
- Ventilator-Induced Lung Injury (VILI)
- Description: Lung injury resulting from mechanical ventilation.
- Causes: High pressures, volumes, and oxygen concentrations.
- Prevention: Using lung-protective strategies and minimising exposure to high oxygen levels.
- Tracheal Injuries
- Description: Damage to the trachea caused by the endotracheal tube.
- Causes: Prolonged intubation, high cuff pressures.
- Prevention: Regular monitoring of cuff pressure, using appropriately sized tubes.
- Oxygen Toxicity
- Description: Lung and tissue damage caused by prolonged exposure to high oxygen concentrations.
- Causes: High FiO2 settings for extended periods.
- Prevention: Reducing FiO2 to the lowest effective level to maintain adequate oxygenation.
- Dysynchrony
- Description: Mismatch between patient’s breathing efforts and ventilator-delivered breaths.
- Causes: Inappropriate ventilator settings, patient agitation.
- Prevention: Adjusting trigger settings, sedation management, and ventilator mode adjustments.
- Airway Obstruction
- Description: Blockage of the airway, often due to secretions or tube displacement.
- Causes: Mucus plugs, kinking of the tube.
- Prevention: Regular suctioning, humidification, and ensuring proper tube positioning.
- Haemodynamic Instability
- Description: Blood pressure fluctuations and cardiac issues related to mechanical ventilation.
- Causes: High intrathoracic pressures, sedation effects.
- Prevention: Careful monitoring and adjusting ventilator settings to minimise cardiovascular impact.
Ethical Considerations
- Patient Consent: Informed consent where possible.
- End-of-Life Care: Decisions regarding continuation or withdrawal of ventilatory support.
