Definition: (The Yellow Pigment Behind Jaundice)
Bilirubin is a yellow compound that is a byproduct of the normal breakdown of red blood cells (RBCs). Red blood cells have a lifespan of about 120 days. When they reach the end of their functional life, they are broken down by the spleen and liver. It is processed by the liver and excreted in bile, which helps in the digestion of fats.
Types of Bilirubin:
- Unconjugated (Indirect) Bilirubin:
- This form of bilirubin is not water-soluble. It is produced from the breakdown of haemoglobin in red blood cells and transported to the liver bound to albumin.
- Conjugated (Direct) Bilirubin:
- In the liver, unconjugated bilirubin is converted into conjugated bilirubin, making it water-soluble. This conversion allows it to be excreted in bile.
Production of Bilirubin:
- Haemoglobin Breakdown:
- When red blood cells reach the end of their lifespan (about 120 days), they are broken down by macrophages in the spleen and liver. The haemoglobin from these cells is split into haem and globin.
- Conversion to Bilirubin:
- The haem component is further broken down into biliverdin and then into unconjugated bilirubin.
- Transport to the Liver:
- Unconjugated bilirubin is transported to the liver bound to albumin in the blood.
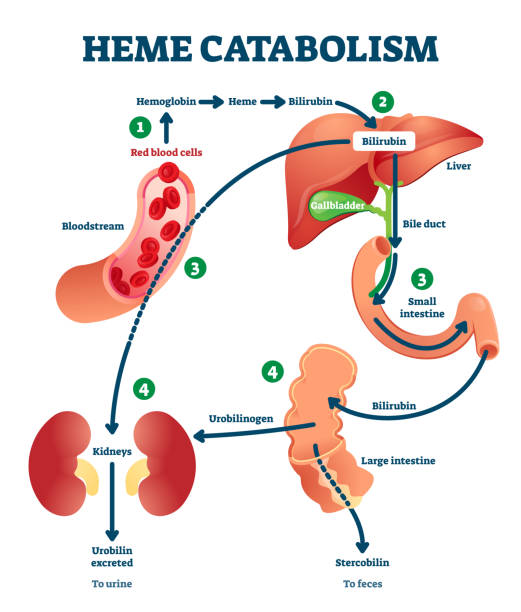
Excretion of Bilirubin:
- Conjugation in the Liver:
- Unconjugated bilirubin is taken up by the liver cells (hepatocytes) where it is conjugated with glucuronic acid to form conjugated bilirubin.
- Secretion into Bile:
- Conjugated bilirubin is secreted into bile canaliculi, which merge to form bile ducts. Bile, containing conjugated bilirubin, is stored in the gallbladder or directly released into the small intestine.
- Excretion in Stool:
- In the intestine, conjugated bilirubin is converted by bacteria into urobilinogen and stercobilin, which are excreted in stool, giving it a brown colour.
- Excretion in Urine:
- Some urobilinogen is reabsorbed into the bloodstream and excreted in urine, giving it a yellow colour.
Causes of Increased Bilirubin Production:
- Haemolysis:
- Increased breakdown of red blood cells due to conditions like haemolytic anaemia or sickle cell disease.
- Liver Dysfunction:
- Conditions like hepatitis, cirrhosis, or liver cancer can impair the liver’s ability to process and excrete bilirubin.
- Obstruction of Bile Ducts:
- Gallstones, tumours, or strictures can block the bile ducts, preventing the excretion of bilirubin. Conjugated bilirubin cannot be excreted into the intestines, leading to a rise in blood levels.
High Bilirubin:
Symptoms of High Bilirubin (Hyperbilirubinaemia):
- Jaundice: Yellowing of the skin and eyes.
- Dark Urine: Due to excess bilirubin being excreted through the kidneys.
- Pale Stools: Lack of bilirubin reaching the intestines.
- Itching (Pruritus): Caused by bilirubin deposits in the skin.
- Fatigue: General tiredness and weakness.
- Abdominal Pain: Especially if the underlying cause is a gallstone or liver disease.
- Nausea and Vomiting: General digestive discomfort.
Diagnosis of High Bilirubin:
- Physical Examination:
- Checking for signs of jaundice and other symptoms.
- Blood Tests:
- Total Bilirubin: Measures both unconjugated and conjugated bilirubin.
- Direct Bilirubin: Measures conjugated bilirubin.
- Indirect Bilirubin: Calculated by subtracting direct bilirubin from total bilirubin.
- Liver Function Tests:
- Tests such as ALT, AST, ALP, and GGT to assess liver function and detect liver damage.
- Imaging Studies:
- Ultrasound: To check for gallstones, liver abnormalities, and bile duct obstructions.
- CT Scan or MRI: For detailed imaging of the liver and bile ducts.
- Liver Biopsy:
- To determine the extent and type of liver damage.
Treatment of High Bilirubin:
- Treat Underlying Cause:
- Medications: For hepatitis or other liver infections.
- Surgery: To remove gallstones or obstructions.
- Lifestyle Changes: Reducing alcohol intake, managing weight, and improving diet.
- Phototherapy:
- Used in newborns with jaundice to help break down bilirubin in the skin.
- Liver Transplant:
- For severe cases of liver failure.
Ammonia: (A Window into Liver Function)
Definition: Ammonia is a toxic byproduct of protein metabolism. It is primarily produced in the intestines and muscles and needs to be converted into a less toxic substance by the liver.
Production of Ammonia:
- Protein Metabolism:
- Ammonia is produced during the breakdown of amino acids in the liver, muscles, and intestines.
- Bacterial Action:
- Intestinal bacteria also produce ammonia during the digestion of proteins.
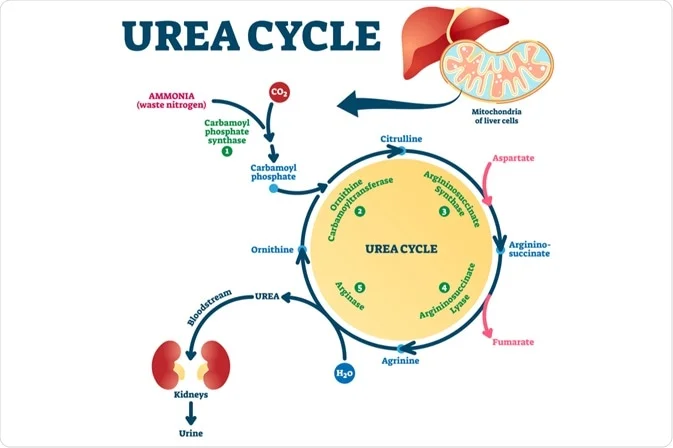
Conversion and Excretion of Ammonia:
- Conversion to Urea: (The Urea Cycle)
- In the liver, ammonia is converted into urea through the urea cycle, making it less toxic and easier to excrete.
- Excretion: (Urea Excretion)
- Urea is then transported to the kidneys, where it is excreted in urine.
Causes:
- Liver Disease: Liver damage or dysfunction can impair the liver’s ability to convert ammonia to urea, leading to a buildup in the bloodstream. This is a common cause of hyperammonemia. Examples include cirrhosis, hepatitis, and fatty liver disease.
- Genetic Disorders: Certain inherited conditions, like urea cycle disorders, affect enzymes involved in the urea cycle, hindering ammonia conversion. These disorders are typically diagnosed in childhood.
- Gastrointestinal Bleeding: Bleeding in the gastrointestinal tract increases the amount of blood and protein in the gut, which bacteria break down into ammonia .
- Renal Failure: Impaired kidney function can reduce the excretion of urea, leading to an accumulation of ammonia in the blood .
- Valproic Acid: An anticonvulsant medication that can lead to hyperammonaemia as a side effect, especially in individuals with underlying metabolic disorders
Symptoms of High Ammonia (Hyperammonaemia):
- Hepatic Encephalopathy: Confusion, altered consciousness, personality changes, and coma.
- Asterixis: Flapping tremor of the hands.
- Fatigue and Weakness: General tiredness.
- Nausea and Vomiting: Digestive discomfort.
- Seizures: In severe cases.
Diagnosis of High Ammonia:
- Blood Tests:
- Serum Ammonia Levels: Direct measurement of ammonia in the blood.
- Liver Function Tests: To assess liver health and function.
- Genetic testing: To screen for urea cycle disorders.Imaging tests: Like ultrasound or CT scan, to evaluate the liver and surrounding structures.
Treatment of High Ammonia:
- Lactulose:
- A non-absorbable sugar that helps reduce ammonia levels by trapping it in the colon and promoting its excretion.
- Antibiotics:
- Rifaximin: To reduce the number of ammonia-producing bacteria in the gut.
- Dietary Changes:
- Protein Restriction: Reducing protein intake to lower ammonia production.
- Liver Transplant:
- For severe cases of liver failure where other treatments are ineffective.
- Dialysis:
- In severe cases, dialysis might be used to remove excess ammonia from the blood.
- Supportive Care:
- Monitoring and managing symptoms of hepatic encephalopathy.
