Blood Pressure
Blood pressure (BP) is the force exerted by circulating blood on the walls of the arteries, which are the major blood vessels in the circulatory system. It is a critical vital sign and an essential indicator of overall cardiovascular health. Blood pressure is usually expressed with two numbers:
- Systolic Blood Pressure (SBP): The pressure in the arteries when the heart contracts and pushes blood out into the arteries.
- Diastolic Blood Pressure (DBP): The pressure in the arteries when the heart is at rest between beats.
Blood pressure is recorded as SBP over DBP, for example, 120/80 mmHg.
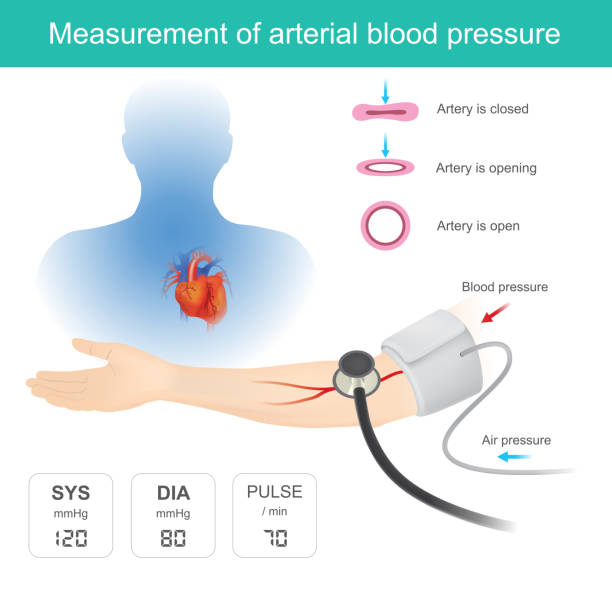
How Blood Pressure is Measured
Blood pressure can be measured using non-invasive and invasive methods:
- Non-Invasive Measurement:
- Manual Sphygmomanometer: Utilises a cuff, an inflatable bladder, a manometer, and a stethoscope.
- Digital Blood Pressure Monitors: Utilise oscillometric or aneroid methods to provide a digital readout.
- Cuff Inflation: A cuff is wrapped around the upper arm and inflated to constrict the arteries, temporarily stopping blood flow.
- Cuff Deflation: The cuff is slowly deflated while listening with a stethoscope (in manual devices) or using a digital readout to detect the points at which blood flow resumes (systolic pressure) and flows freely (diastolic pressure).
2. Invasive Measurement:
- Arterial Line (A-line): Involves the insertion of a catheter into an artery, typically the radial or femoral artery. This provides continuous, real-time blood pressure readings and is used in critical care settings.
- Procedure: The catheter is connected to a pressure transducer that converts the pressure into an electrical signal displayed on a monitor.
Normal Blood Pressure Ranges (UK)
The National Institute for Health and Care Excellence (NICE) guidelines provide the following categories for blood pressure in adults:
- Optimal: Less than 120/80 mmHg
- Normal: 120/80 mmHg to 129/84 mmHg
- High-Normal: 130/85 mmHg to 139/89 mmHg
- Hypertension Stage 1: 140/90 mmHg to 159/99 mmHg
- Hypertension Stage 2: 160/100 mmHg to 179/119 mmHg
- Hypertensive Crisis: 180/120 mmHg or higher, requiring immediate medical attention
Factors Affecting Blood Pressure
- Age: Blood pressure generally increases with age due to the gradual stiffening of arteries.
- Diet: High salt intake can elevate blood pressure. Diets rich in fruits, vegetables, and low-fat dairy products can help lower blood pressure.
- Weight: Obesity increases the risk of developing hypertension.
- Physical Activity: Regular physical activity can help lower blood pressure.
- Alcohol and Tobacco Use: Excessive alcohol consumption and smoking can raise blood pressure.
- Stress: Chronic stress can contribute to high blood pressure.
- Genetics: A family history of hypertension increases the risk.
- Health Conditions: Conditions like diabetes, kidney disease, and high cholesterol can impact blood pressure.
Significance of Blood Pressure
- Hypertension (High Blood Pressure):
- Risks: Increases the risk of cardiovascular diseases, such as heart disease, stroke, kidney disease, and vascular dementia.
- Management: Lifestyle modifications (diet, exercise), medications, and regular monitoring.
2. Hypotension (Low Blood Pressure):
- Risks: Can cause dizziness, fainting, and, in severe cases, shock.
- Management: May involve increasing fluid and salt intake, wearing compression stockings, and treating underlying conditions.
Monitoring and Management
- Home Monitoring: Regular monitoring at home can help manage hypertension and understand how lifestyle changes affect blood pressure. It is recommended to use validated home blood pressure monitors and follow the guidance provided by healthcare professionals.
- Medical Check-ups: Regular visits to a healthcare provider for blood pressure checks are essential, especially for individuals with a history of hypertension or other cardiovascular risks.
- Medications: Several classes of medications are used to manage high blood pressure, including:
Diuretics: Help reduce blood volume by increasing urine production.
- Example: Bendroflumethiazide (Thiazide diuretics)
2. ACE Inhibitors: Relax blood vessels by inhibiting the formation of a hormone that narrows blood vessels.
- Example: Ramipril
3. Angiotensin II Receptor Blockers (ARBs): Block the effects of angiotensin II, a hormone that can raise blood pressure.
- Example: Losartan
4. Beta-blockers: Reduce the workload on the heart and open blood vessels.
- Example: Bisoprolol
5. Calcium Channel Blockers: Relax blood vessels and reduce heart rate.
- Example: Amlodipine
6. Others: Such as alpha-blockers, central agonists, and vasodilators.
- Example: Doxazosin (alpha-blocker)
Clinical Practice Guidelines
The management of blood pressure in the UK follows guidelines from NICE and other professional bodies. Key points include:
- Lifestyle Interventions: Emphasize the importance of dietary changes (reducing salt intake, increasing fruit and vegetable consumption), regular physical activity, weight loss, and moderation of alcohol intake.
- Medication Management: Initiating and titrating antihypertensive medications based on individual patient profiles, comorbidities, and blood pressure targets.
- Regular Monitoring: Encouraging regular home monitoring and routine clinical reviews to assess treatment effectiveness and adherence.
Summary
Blood pressure is a crucial measure of cardiovascular health, reflecting the force of blood against arterial walls during heartbeats and rest periods. Maintaining a normal blood pressure range through lifestyle choices, regular monitoring, and, if necessary, medication, is essential for reducing the risk of serious health conditions such as heart disease, stroke, and kidney disease. Following UK-specific guidelines and recommendations helps ensure optimal management and prevention of hypertension and its associated complications.
