Cardiomyopathy: When the Heart Muscle Weakens
Cardiomyopathy refers to diseases of the heart muscle where the myocardium becomes enlarged, thick, or rigid. In rare cases, the muscle tissue is replaced with scar tissue. These changes can impair the heart’s ability to pump blood effectively, potentially leading to heart failure or irregular heartbeats (arrhythmias)
Types of Cardiomyopathy:
- Dilated Cardiomyopathy (DCM)
- Hypertrophic Cardiomyopathy (HCM)
- Restrictive Cardiomyopathy (RCM)
- Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
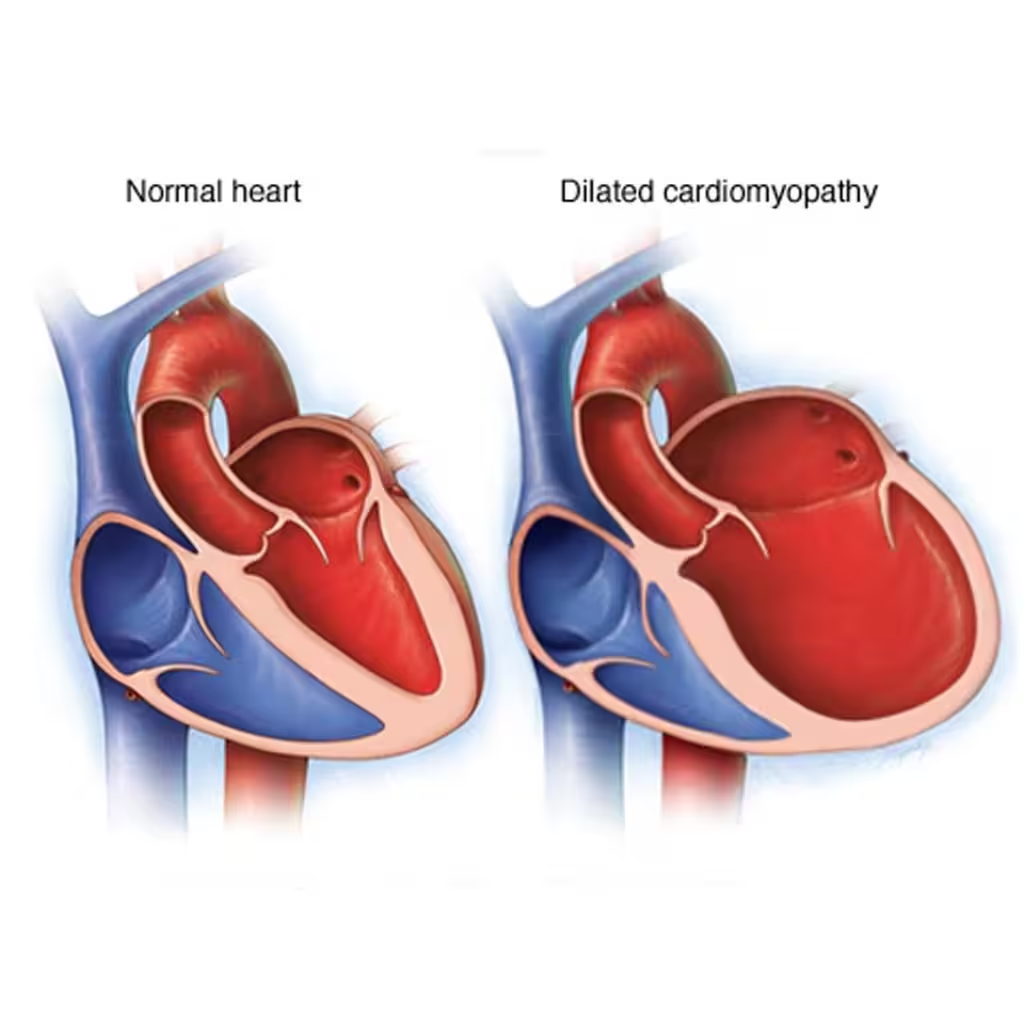
- Dilated Cardiomyopathy (DCM):
- Description: The left ventricle becomes enlarged and cannot contract effectively. This reduces the heart’s pumping efficiency.
- Causes: Can be genetic, or result from coronary artery disease, alcohol abuse, infections, or exposure to toxins.
- Symptoms: Shortness of breath, fatigue, swollen legs and feet, arrhythmias, and chest pain.
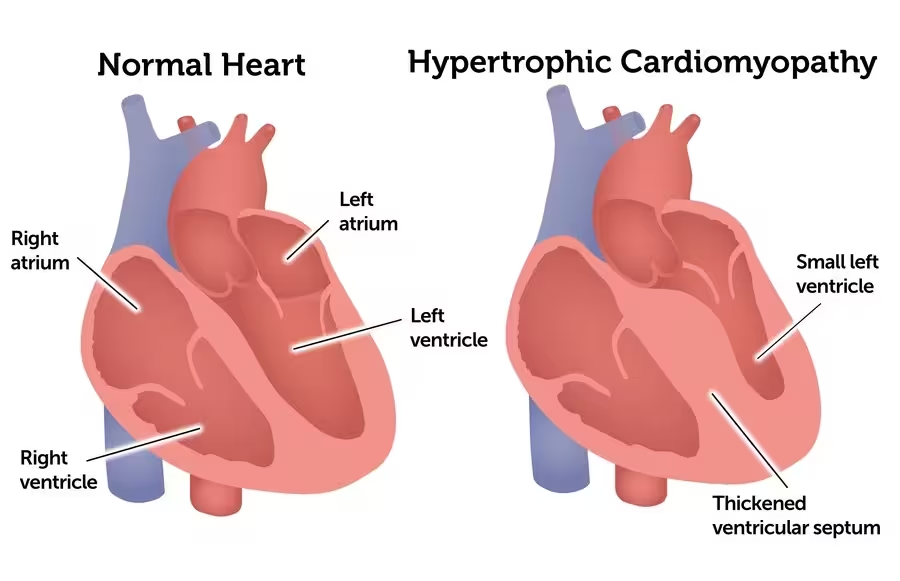
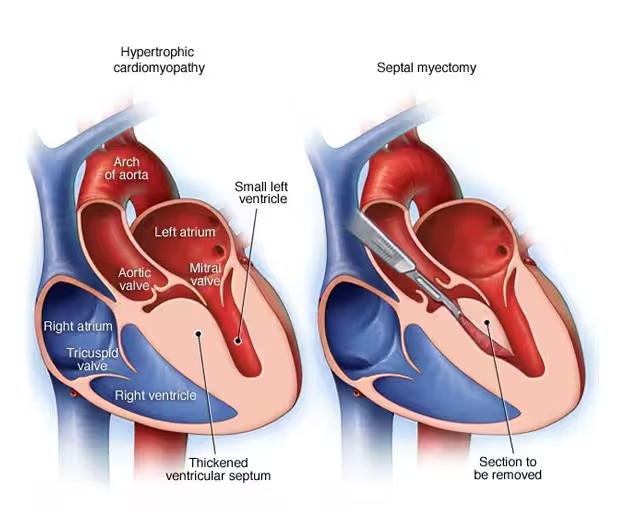
2. Hypertrophic Cardiomyopathy (HCM):
- Description: The heart muscle becomes abnormally thick, making it harder for the heart to pump blood. The thickening often occurs in the interventricular septum.
- Causes: Usually genetic, resulting from mutations in the genes responsible for heart muscle proteins.
- Symptoms: Shortness of breath, chest pain, palpitations, fainting (syncope), and in severe cases, sudden cardiac arrest.
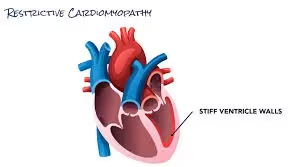
3. Restrictive Cardiomyopathy (RCM):
- Description: The heart muscle becomes rigid and less elastic, preventing the heart chambers from filling properly with blood.
- Causes: Can be idiopathic or caused by diseases such as amyloidosis, sarcoidosis, or hemochromatosis.
- Symptoms: Shortness of breath, fatigue, swollen legs and feet, and arrhythmias.
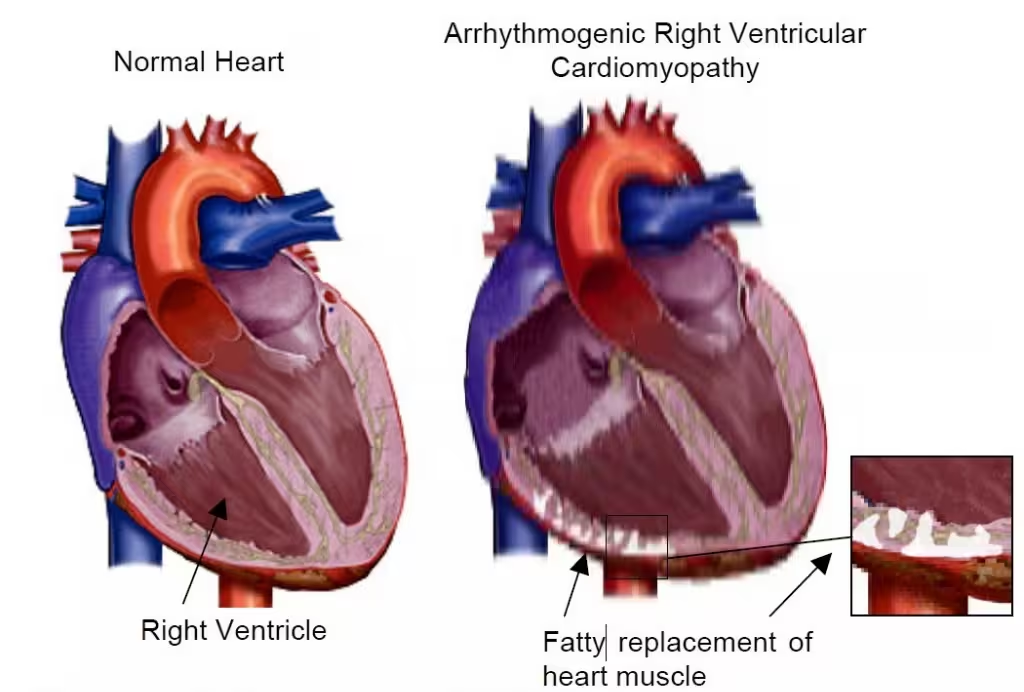
4. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC):
- Description: Fat and fibrous tissue replaces the muscle in the right ventricle, disrupting the heart’s electrical signals and leading to arrhythmias.
- Causes: Typically genetic, often involving mutations in desmosomal proteins.
- Symptoms: Palpitations, fainting, and in severe cases, sudden cardiac death.
Symptoms: The symptoms of cardiomyopathy can vary depending on the type and severity but often include:
- Shortness of breath, especially during exertion or when lying flat
- Fatigue
- Swelling in the legs, ankles, and feet
- Chest pain, particularly after physical exertion or heavy meals
- Palpitations or irregular heartbeats
- Dizziness or fainting
Diagnosis: Diagnosis of cardiomyopathy involves a combination of medical history, physical examination, and various diagnostic tests:
- Medical History and Physical Examination:
- Detailed patient history to identify symptoms and risk factors.
- Physical examination to check for signs of heart failure, such as swelling or abnormal heart sounds.
- Imaging and Diagnostic Tests:
- Echocardiogram: To assess heart structure and function.
- Electrocardiogram (ECG): To detect abnormal heart rhythms and electrical activity.
- Cardiac MRI: Provides detailed images of the heart’s structure and can identify scarring or fibrosis.
- Chest X-ray: To detect heart enlargement and fluid buildup in the lungs.
- Blood Tests: To check for markers of heart failure and other underlying conditions.
- B-type Natriuretic Peptide (BNP) or NT-proBNP: Elevated levels indicate heart failure and are useful in diagnosing and assessing the severity of cardiomyopathy.
- Troponin:Measures cardiac muscle damage and helps rule out myocardial infarction.
- Genetic Testing: Recommended for patients with a family history of cardiomyopathy.
- Recommended for patients with a family history of cardiomyopathy or when cardiomyopathy is diagnosed at a young age. Genetic testing can identify mutations in specific genes associated with different types of cardiomyopathy, particularly hypertrophic and arrhythmogenic right ventricular cardiomyopathy. Identifying a genetic cause can help guide treatment and inform family members about their potential risk.
Management: Management of cardiomyopathy aims to control symptoms, improve quality of life, and reduce the risk of complications. The approach includes:
- Medical Treatment:
- Medications: Beta-blockers, ACE inhibitors, ARBs, diuretics, and anti-arrhythmic drugs to manage symptoms and prevent complications.
- Anticoagulants: To reduce the risk of blood clots in patients with atrial fibrillation or other risk factors.
- Device Therapy:
- Implantable Cardioverter Defibrillator (ICD): For patients at risk of sudden cardiac death due to arrhythmias.
- Pacemakers: To manage bradycardia (slow heart rate) or heart block.
- Cardiac Resynchronisation Therapy (CRT): For patients with heart failure and dyssynchrony in ventricular contraction.
- Surgical Options:
- Septal Myectomy: For patients with obstructive hypertrophic cardiomyopathy, where part of the thickened septum is removed.
- Heart Transplant: For patients with end-stage heart failure not responding to other treatments.
- Left Ventricular Assist Device (LVAD): As a bridge to transplant or for long-term support in select patients.
- Lifestyle Modifications:
- Dietary Changes: Low-sodium diet to reduce fluid retention.
- Exercise: Tailored exercise programmes to improve cardiovascular health.
- Smoking Cessation: To improve overall heart health and reduce disease progression.
- Alcohol Moderation: Limiting alcohol intake to prevent further heart damage.
Conclusion: Cardiomyopathy is a serious condition that requires a comprehensive approach to management. Early recognition and treatment are crucial to improving outcomes and quality of life for patients.
References:
