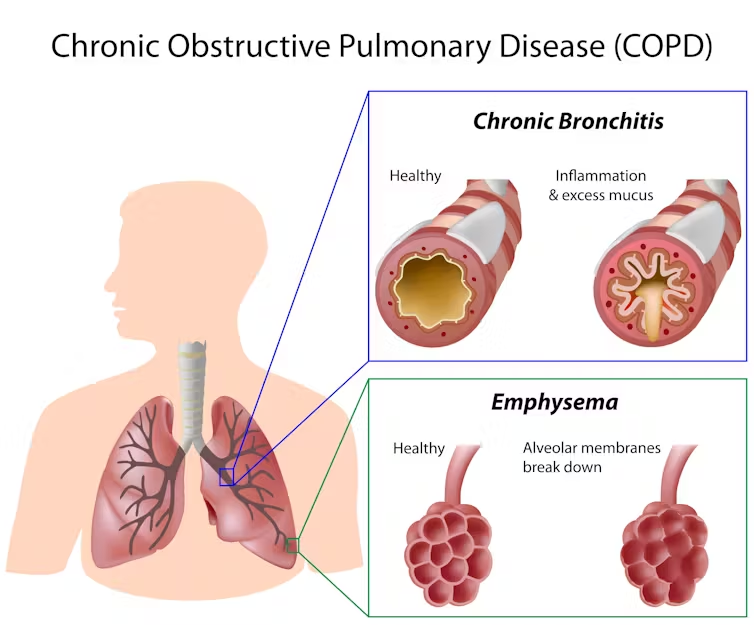
Chronic Obstructive Pulmonary Disease (COPD) is an umbrella ☂️ term for progressive inflammatory lung diseases that cause airflow limitation due to airway and/or alveolar abnormalities. It typically involves a combination of chronic bronchitis and emphysema, primarily caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke.
Causes
- Smoking: The primary cause, accounting for the majority of cases.
- Air pollution: Long-term exposure to air pollution, chemical fumes, and dust.
- Genetics: A rare genetic disorder known as alpha-1 antitrypsin deficiency can cause COPD.
Symptoms
- Chronic cough: Often referred to as “smoker’s cough.” this is a persistent cough that produces mucus.
- Sputum production: Producing large amounts of mucus.
- Shortness of breath: Especially during physical activities.
- Wheezing: A whistling sound when breathing.
- Chest tightness: Discomfort or pain in the chest.
- Frequent respiratory infections: Including colds, flu, and pneumonia.
- Fatigue: Feeling tired and lacking energy.
Diagnosis
- Spirometry: A lung function test that measures the amount of air you can inhale and exhale, and how quickly you can exhale. It is the gold standard for diagnosing COPD.
- Chest X-ray: Helps identify emphysema and rule out other lung problems.
- CT scan: Provides detailed images of the lungs.
- Arterial blood gas analysis: Measures how well your lungs are bringing oxygen into your blood and removing carbon dioxide.
Stages
COPD is typically classified into four stages based on the severity of symptoms and lung function:
- Mild (Stage 1): Slight airflow limitation and chronic cough with sputum production.
- Moderate (Stage 2): Worsening airflow limitation, shortness of breath with exertion, and cough with sputum production.
- Severe (Stage 3): Further worsening of airflow limitation, increased shortness of breath, and frequent exacerbations.
- Very severe (Stage 4): Severe airflow limitation, significantly impaired quality of life, and life-threatening exacerbations.
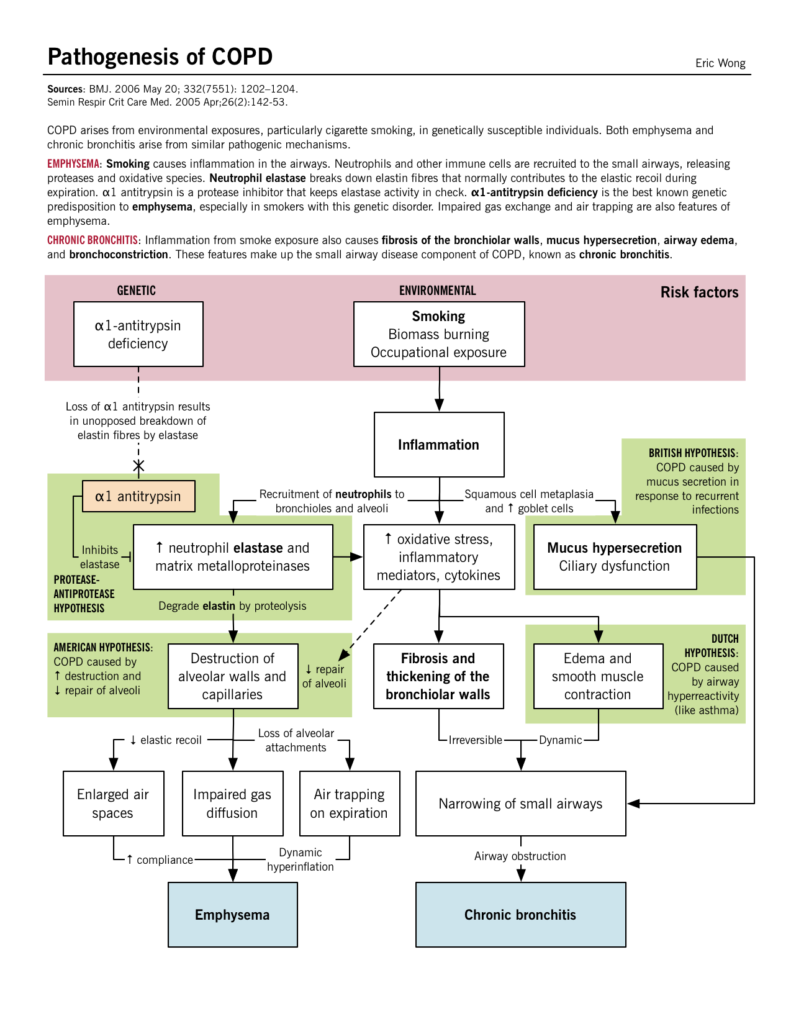
Pathophysiology of COPD
- Inhalation of Smoke Particles:
- When you inhale smoke (from cigarettes, pollution, etc.), tiny particles and chemicals in the smoke enter your lungs.
- Initial Immune Response:
- The inhaled particles cause epithelial cell injury in the airways and alveoli.
- Epithelial cells release pro-inflammatory mediators that attract immune cells to the lungs.
- Infiltration of Immune Cells:
- Two key types of immune cells are recruited to the lungs: macrophages and neutrophils.
- Macrophages: These are large white blood cells that “eat” and digest foreign particles, bacteria, and dead cells.
- Neutrophils: These are a type of white blood cell that helps fight infection by ingesting microorganisms and releasing enzymes.
- Release of Inflammatory Mediators:
- These immune cells release various substances in response to smoke particles:
- Cytokines: Small proteins that signal other immune cells to come to the site of inflammation.
- Chemokines: A subtype of cytokines that specifically attract more immune cells to the site of infection or injury.
- Elastases: Enzymes that break down proteins, including elastin, which is a key component of the lung’s connective tissue.
- These immune cells release various substances in response to smoke particles:
- Inflammation and Damage:
- The release of these substances leads to inflammation in the lung tissue.
- Over time, the continuous recruitment of immune cells and release of elastases causes damage to the lung parenchyma (the functional tissue of the lung).
- Elastases, in particular, can break down the elastin fibers in the lung, leading to a loss of elasticity and structural damage.
- Chronic Inflammation:
- If exposure to smoke continues, the inflammation becomes chronic.
- This ongoing inflammation further damages the lung tissue and impairs lung function.
- Progression to Disease:
- The cumulative damage from chronic inflammation can lead to diseases such as chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema.
- In emphysema, the destruction of alveoli (air sacs) reduces the surface area for gas exchange, making it difficult to breathe.
- In chronic bronchitis, the airways become inflamed and produce excess mucus, which also obstructs airflow.
Management of COPD
Lifestyle Modifications
- Smoking Cessation:
- The most crucial step in managing COPD is to stop smoking. Resources include nicotine replacement therapies, prescription medications, and behavioral support.
- Avoiding Irritants:
- Reducing exposure to indoor and outdoor pollutants, occupational dust, and chemicals is important.
Pharmacotherapy
- Bronchodilators:
- Short-acting bronchodilators (SABAs and SAMAs): To open the airways and for quick relief.
- Salbutamol (SABA): 100-200 mcg inhaled every 4-6 hours as needed.
- Ipratropium (SAMA): 20-40 mcg inhaled 3-4 times daily.
- Long-acting bronchodilators (LABAs and LAMAs): For maintenance therapy.
- Salmeterol (LABA): 50 mcg inhaled twice daily.
- Formoterol (LABA): 12 mcg inhaled twice daily.
- Tiotropium (LAMA): 18 mcg inhaled once daily.
- Aclidinium (LAMA): 322 mcg inhaled twice daily.
- Short-acting bronchodilators (SABAs and SAMAs): To open the airways and for quick relief.
- Inhaled Corticosteroids (ICS): For reducing inflammation
- Used in combination with long-acting bronchodilators for patients with frequent exacerbations.
- Beclometasone/Formoterol: 100/6 mcg, two puffs twice daily.
- Fluticasone/Salmeterol: 250/50 mcg, one inhalation twice daily.
- Used in combination with long-acting bronchodilators for patients with frequent exacerbations.
- Combination Inhalers:
- Combining bronchodilators and corticosteroids for enhanced efficacy.
- Fluticasone/Salmeterol (Seretide): 250/50 mcg, one inhalation twice daily.
- Budesonide/Formoterol (Symbicort): 160/4.5 mcg, two inhalations twice daily.
- Combining bronchodilators and corticosteroids for enhanced efficacy.
- Phosphodiesterase-4 Inhibitors:
- Used in severe COPD with chronic bronchitis to reduce inflammation.
- Roflumilast: 500 mcg orally once daily.
- Used in severe COPD with chronic bronchitis to reduce inflammation.
- Mucolytics: (To thin mucus and ease expectoration.)
- To help thin and clear mucus from the airways.
- Carbocisteine: 375 mg capsules, two capsules three times daily initially, then reduced to one capsule four times daily.
- To help thin and clear mucus from the airways.
Managing Exacerbations
- Acute Exacerbations:
- Managed with bronchodilators, systemic corticosteroids, and antibiotics if bacterial infection is suspected.
- Severe exacerbations may require hospital admission and advanced therapies like non-invasive ventilation.
Ventilatory Support
- Non-invasive ventilation (NIV): First-line for patients with respiratory acidosis or severe dyspnoea.
- Invasive mechanical ventilation: For those who fail NIV or have severe respiratory failure.
Advanced Interventions
- Surgical Options:
- Lung Volume Reduction Surgery (LVRS): For selected patients with severe emphysema.
- Bullectomy: For patients with large bullae.
- Lung Transplantation: In end-stage COPD for eligible patients.
- Palliative Care:
- Focused on managing symptoms and improving the quality of life in advanced stages.
Nursing Management for COPD
Nursing management for COPD involves comprehensive care to alleviate symptoms, prevent complications, and improve the quality of life for patients. Key aspects include:
- Assessment:
- Monitor respiratory status, including breath sounds, respiratory rate, and oxygen saturation.
- Assess for signs of hypoxia and respiratory distress.
- Medication Administration:
- Ensure adherence to prescribed bronchodilators, corticosteroids, and other medications.
- Educate patients on correct inhaler techniques.
- Oxygen Therapy:
- Administer supplemental oxygen as prescribed, ensuring correct flow rates.
- Monitor for signs of oxygen toxicity and adjust therapy as needed.
- Patient Education:
- Teach breathing exercises, such as pursed-lip breathing and diaphragmatic breathing.
- Provide information on smoking cessation and avoiding lung irritants.
- Nutritional Support:
- Encourage a balanced diet to maintain optimal weight and muscle strength.
- Offer small, frequent meals to prevent breathlessness during eating.
- Activity Management:
- Promote regular, moderate exercise to improve cardiovascular fitness and muscle strength.
- Assist in developing an activity plan that includes rest periods to prevent fatigue.
- Psychosocial Support:
- Address anxiety, depression, and other psychological issues related to COPD.
- Provide support groups and counseling resources.
- Emergency Management:
- Educate patients and families on emergency signs and symptoms, and ensure they know when to seek urgent medical care.
The NICE guideline [NG115]
The NICE guideline [NG115] provides detailed recommendations for diagnosing and managing Chronic Obstructive Pulmonary Disease (COPD) in people over 16. Key recommendations include:
- Diagnosis:
- Use of spirometry to confirm diagnosis.
- Assessment of symptoms such as breathlessness, chronic cough, and sputum production.
- Pharmacological Management:
- Bronchodilators: Short-acting and long-acting for symptom relief.
- Inhaled Corticosteroids (ICS): For patients with frequent exacerbations.
- Combination Inhalers: Combining bronchodilators and ICS for enhanced control.
- Oral Therapies: Mucolytics, and phosphodiesterase-4 inhibitors.
- Non-Pharmacological Management:
- Pulmonary Rehabilitation: Exercise training, education, and behavioral modification.
- Oxygen Therapy: For patients with chronic hypoxemia.
- Nutritional Support: Dietary advice to maintain optimal weight and nutrition.
- Vaccinations: Annual influenza and pneumococcal vaccines.
- Exacerbation Management:
- Acute Exacerbations: Use of bronchodilators, corticosteroids, and antibiotics.
- Severe Exacerbations: Hospital admission if necessary, with advanced therapies such as non-invasive ventilation.
- Multidisciplinary Care:
- Involvement of physiotherapists, occupational therapists, and palliative care teams.
- Emphasis on holistic care addressing physical, psychological, and social aspects.
- Patient Education and Self-Management:
- Educating patients about their condition.
- Encouraging self-management plans to handle exacerbations.
- Monitoring and Follow-Up:
- Regular review of treatment effectiveness and adjustment as necessary.
- Monitoring for disease progression and complications.
- Advanced Treatments:
- Surgical Options: Lung volume reduction surgery, bullectomy, and lung transplantation for selected patients.
