Clotting factors, also known as coagulation factors, are proteins in the blood that work together to form a blood clot. This process, known as coagulation, is essential for stopping bleeding when an injury occurs. Clotting factors are part of a complex cascade of events, each activating the next in a precise sequence to ensure efficient blood clot formation.
Clotting Factors
Clotting factors are proteins in blood plasma that help form blood clots to stop bleeding after an injury. There are 13 clotting factors that are numbered based on when they were discovered, but some factors have more than one name.
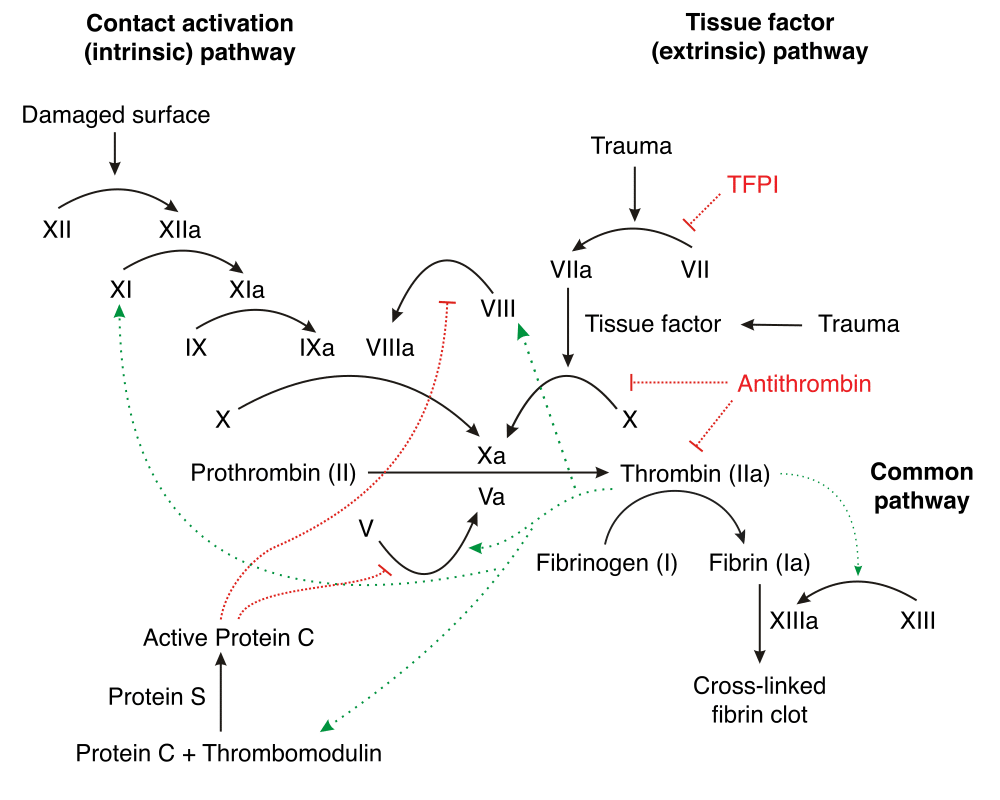
These factors interact in a cascade that is divided into three pathways: the intrinsic, extrinsic, and common pathways, all leading to the formation of a stable blood clot.
- Factor I (Fibrinogen)
- Factor II (Prothrombin)
- Factor III (Tissue Factor)
- Factor IV (Calcium ions)
- Factor V (Proaccelerin)
- Factor VII (Proconvertin)
- Factor VIII (Antihemophilic Factor)
- Factor IX (Christmas Factor)
- Factor X (Stuart-Prower Factor)
- Factor XI (Plasma Thromboplastin Antecedent)
- Factor XII (Hageman Factor)
- Factor XIII (Fibrin-stabilizing Factor)
The Clotting Cascade–
These factors interact in a cascade that is divided into three pathways: the intrinsic, extrinsic, and common pathways, all leading to the formation of a stable blood clot.
- Intrinsic Pathway: Initiated by damage inside the vascular system and is activated by internal trauma. It involves factors XII, XI, IX, and VIII.
- Extrinsic Pathway: Triggered by external trauma that causes blood to escape from the vascular system, involving factor VII and tissue factor.
- Common Pathway: Where both pathways converge, involving factors X, V, II (prothrombin), and I (fibrinogen), leading to the formation of a stable blood clot.
Clotting Abnormalities
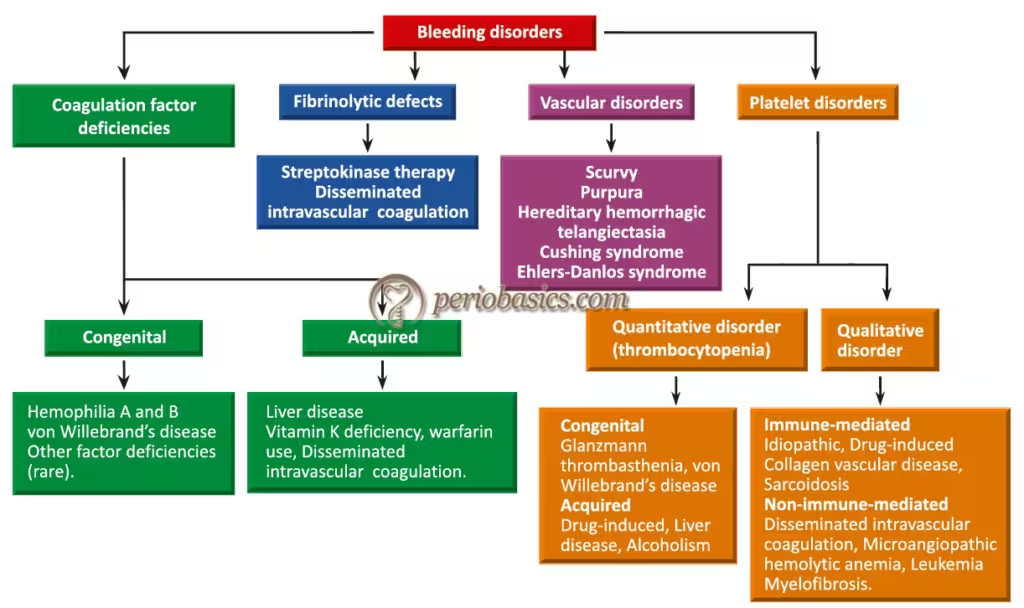
Clotting abnormalities refer to disorders that affect the normal process of blood coagulation. This process is crucial for stopping bleeding when a blood vessel is injured. Abnormalities in clotting can lead to either excessive bleeding (hemorrhagic disorders) or excessive clotting (thrombotic disorders).
Types of Clotting Abnormalities
- Hemorrhagic Disorders
- Definition: Conditions that result in excessive bleeding due to an inability to form effective blood clots.
- Causes: This can be due to genetic factors, deficiencies in clotting factors, or acquired conditions.
- Examples:
- Haemophilia: A genetic disorder caused by the deficiency of clotting factors VIII (Haemophilia A) or IX (Haemophilia B).
- Von Willebrand Disease: A genetic disorder caused by a deficiency or dysfunction of the von Willebrand factor, which helps platelets stick to the blood vessel wall and carry factor VIII.
- Vitamin K Deficiency: Vitamin K is essential for synthesizing clotting factors II, VII, IX, and X. Deficiency can lead to bleeding tendencies.
2. Thrombotic Disorders
- Definition: Conditions that result in excessive clot formation, leading to blockages in blood vessels.
- Causes: Can be genetic or acquired and involve abnormalities in clotting factors or the fibrinolytic system.
- Examples:
- Deep Vein Thrombosis (DVT): Formation of a blood clot in a deep vein, usually in the legs, which can lead to pulmonary embolism if the clot dislodges and travels to the lungs.
- Factor V Leiden: A genetic mutation that increases the risk of abnormal blood clotting.
- Antiphospholipid Syndrome: An autoimmune disorder that causes an increased risk of blood clots due to the presence of antiphospholipid antibodies.
Mechanisms of Clotting Abnormalities
- Deficiencies in Clotting Factors:
- Inherited Deficiencies: Conditions such as haemophilia are caused by mutations in the genes responsible for producing clotting factors.
- Acquired Deficiencies: Liver disease, vitamin K deficiency, and certain medications (e.g., warfarin) can lead to reduced levels of clotting factors.
- Platelet Dysfunction:
- Quantitative Disorders: Thrombocytopenia (low platelet count) can result from bone marrow disorders, autoimmune diseases, or certain medications.
- Qualitative Disorders: Platelet function disorders, such as Glanzmann’s thrombasthenia, affect the ability of platelets to aggregate and form a clot.
- Hypercoagulability:
- Genetic Mutations: Mutations such as Factor V Leiden and prothrombin gene mutation can increase the risk of thrombosis.
- Acquired Conditions: Conditions such as cancer, pregnancy, prolonged immobility, and certain medications (e.g., oral contraceptives) can increase the risk of abnormal clotting.
Clinical Manifestations
- Hemorrhagic Disorders:
- Bleeding: Easy bruising, spontaneous bleeding (e.g., nosebleeds, gum bleeding), prolonged bleeding from cuts, and heavy menstrual periods.
- Joint and Muscle Bleeding: Common in severe haemophilia, leading to joint pain and swelling.
- Thrombotic Disorders:
- DVT Symptoms: Swelling, pain, and redness in the affected limb.
- Pulmonary Embolism: Sudden shortness of breath, chest pain, and rapid heart rate.
- Arterial Thrombosis: This can lead to conditions such as stroke or myocardial infarction (heart attack).
Treatment
- Hemorrhagic Disorders:
- Clotting Factor Replacement: For conditions like haemophilia, intravenous administration of the missing clotting factor.
- Desmopressin (DDAVP): Used to treat mild haemophilia A and von Willebrand disease by stimulating the release of stored von Willebrand factor and factor VIII.
- Vitamin K Supplementation: For vitamin K deficiency.
- Thrombotic Disorders:
- Anticoagulants: Medications such as heparin, warfarin, and direct oral anticoagulants (DOACs) to prevent further clotting.
- Thrombolytics: Medications to dissolve existing clots, used in emergencies like stroke or myocardial infarction.
- Lifestyle Changes: Encouraging regular exercise, weight management, and avoiding prolonged immobility.
Clotting products
Types, Indications, and Administration
- Fresh Frozen Plasma (FFP)
- Indications: Massive transfusions, liver disease, coagulopathies, reversal of warfarin overdose.
- Administration: Given intravenously, typically dosed at 10-20 mL/kg, depending on the clinical scenario.
- Cryoprecipitate
- Indications: Fibrinogen deficiency, Disseminated Intravascular Coagulation (DIC), haemophilia A (if factor concentrates are unavailable).
- Administration: Each unit is pooled and administered intravenously. Dosage typically aims for a fibrinogen level >1.0 g/L.
- Platelet Concentrates
- Indications: Thrombocytopenia, platelet function disorders, massive transfusion protocols.
- Administration: Infused intravenously. The standard dose is one adult therapeutic dose (ATD), typically raising platelet count by 20-40 x 10^9/L.
- Prothrombin Complex Concentrates (PCCs)
- Indications: Warfarin reversal, haemophilia B, factor II, VII, IX, and X deficiencies.
- Administration: Intravenous infusion, dose depends on the indication and severity of deficiency. For warfarin reversal, typical doses are 25-50 units/kg.
- Recombinant Coagulation Factors
- Indications: Haemophilia A (Factor VIII), Haemophilia B (Factor IX).
- Administration: Intravenous injection, dosing based on patient weight and severity of bleeding. For example, Factor VIII dosage may be 20-40 IU/kg for minor bleeding.
- Fibrin Sealants and Thrombin
- Indications: Surgical bleeding control, adjunct to haemostasis during surgery.
- Administration: Applied topically directly to the bleeding site.
