Definition:
A colectomy is a surgical procedure involving the removal of all or part of the colon, also known as the large intestine. This surgery is typically performed to treat various conditions affecting the colon, such as colorectal cancer, inflammatory bowel disease, diverticulitis, and bowel obstruction.
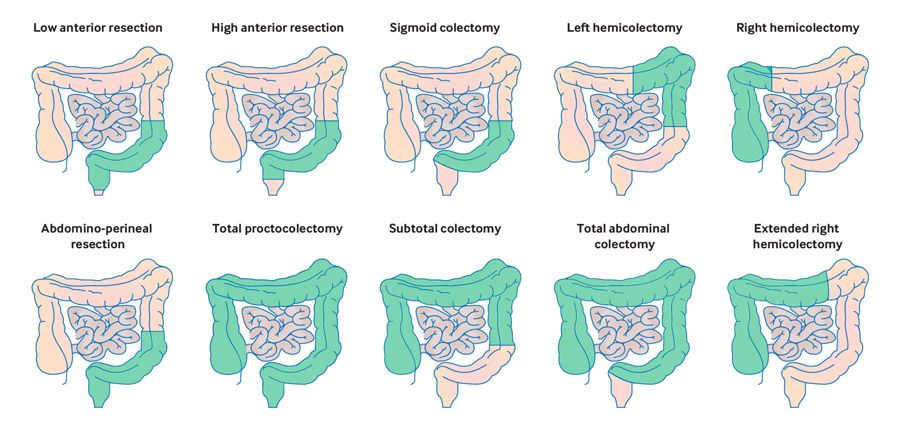
Types of Colectomy:
- Total Colectomy:
- Involves the removal of the entire colon.
2. Partial Colectomy:
- Involves the removal of a segment of the colon. This can be further categorised into:
- Right Hemicolectomy: Removal of the ascending colon.
- Left Hemicolectomy: Removal of the descending colon.
- Sigmoid Colectomy: Removal of the sigmoid colon.
- Segmental Colectomy: Removal of a specific segment of the colon.
3. Proctocolectomy:
- Involves the removal of both the colon and the rectum.
4. Subtotal Colectomy:
- Removal of part of the colon but not the entire colon.
Indications:
- Colorectal Cancer: To remove cancerous growths in the colon.
- Inflammatory Bowel Disease (IBD): For severe cases of Crohn’s disease or ulcerative colitis that do not respond to medical treatment.
- Diverticulitis: To treat inflammation or infection of diverticula, especially in recurrent or complicated cases.
- Bowel Obstruction: To relieve a blockage in the colon.
- Polyps: To remove large or numerous polyps that cannot be managed endoscopically.
Surgical Techniques:
- Open Colectomy:
- A traditional surgery involving a large abdominal incision to access the colon.
2. Laparoscopic Colectomy:
- A minimally invasive approach using several small incisions and a camera (laparoscope) to guide the surgery. This method typically results in faster recovery, less pain, and smaller scars.
3. Robot-Assisted Colectomy:
- Similar to laparoscopic surgery but with the addition of robotic instruments controlled by the surgeon for greater precision.
Procedure:
- Preoperative Preparation:
- Bowel Preparation: Patients may undergo bowel preparation to clear the intestines. This involves taking laxatives and/or enemas to empty the colon.
- Fasting: Patients are usually required to fast for a specific period before surgery.
- Antibiotics: Administered to reduce the risk of infection.
- Medical Assessment: Includes blood tests, imaging studies (e.g., CT scan, MRI), and sometimes colonoscopy to evaluate the extent of the disease.
2. Surgical Steps:
- Anaesthesia: General anaesthesia is administered.
- Incisions: Depending on the technique (open, laparoscopic, or robotic), appropriate incisions are made.
- Colon Removal: The affected part of the colon is identified and removed. Nearby lymph nodes may also be removed if cancer is present.
- Reconstruction: The remaining sections of the colon are reconnected (anastomosis). A temporary or permanent colostomy or ileostomy may be created. This involves creating an opening (stoma) on the abdominal wall to allow waste to exit the body.
3. Postoperative Care:
- Monitoring: Patients are closely monitored in the hospital for signs of complications such as bleeding, infection, or anastomotic leak.
- Pain Management: Pain relief through medications, including opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and local anaesthetics.
- Nutrition: Initially, nutrition is provided intravenously or through a feeding tube. Gradual reintroduction of oral intake starting with clear liquids, then progressing to solid foods as tolerated.
- Mobilisation: Early mobilisation to prevent complications such as blood clots and pneumonia. Patients are encouraged to get out of bed and walk as soon as possible after surgery.
- Wound Care: Instructions on how to care for the surgical incision site to prevent infection and promote healing.
Complications:
- Infection: Risk of wound infections or intra-abdominal infections.
- Anastomotic Leak: A leak at the site where the colon is reconnected can lead to peritonitis and sepsis.
- Bleeding: Risk of bleeding during or after the surgery, which may require blood transfusions.
- Bowel Obstruction: Due to adhesions or scar tissue forming post-surgery.
- Nutritional Deficiencies: Especially if a large portion of the colon is removed, affecting absorption of nutrients and fluids.
Recovery:
- Hospital Stay: Varies depending on the type of colectomy and patient’s overall health, typically ranging from 3 to 7 days.
- At Home: Full recovery can take several weeks to months. Patients are advised to follow a diet plan and gradually return to normal activities.
- Follow-Up: Regular follow-up appointments to monitor recovery and detect any potential complications early. This may include blood tests, imaging studies, and colonoscopy if needed.
Outcomes:
- Prognosis: Depends on the underlying condition being treated. For cancer, the stage at which the cancer was diagnosed and treated significantly affects prognosis.
- Quality of Life: For benign conditions like diverticulitis or IBD, a colectomy can greatly improve quality of life and manage symptoms effectively.
References:
