A comprehensive abdominal assessment is crucial in identifying potential abnormalities or underlying conditions within the abdominal cavity. This assessment involves a systematic approach, including patient history, inspection, auscultation, percussion, and palpation, each targeting specific signs and symptoms.
Abdominal Quadrants
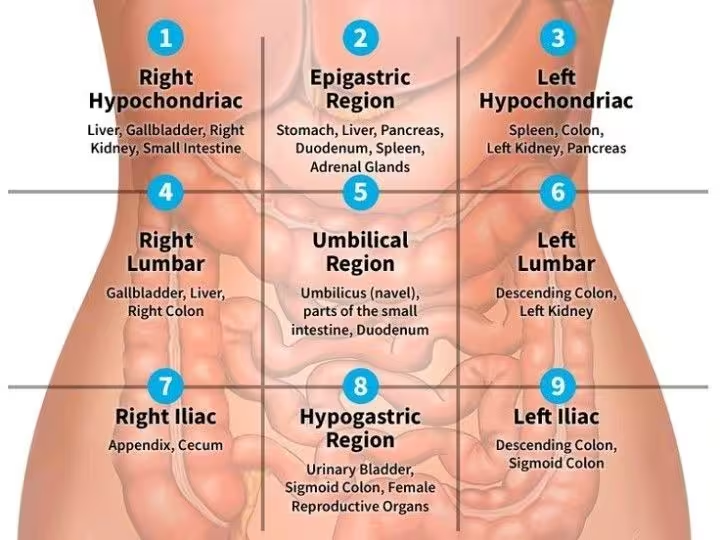
The abdomen is divided into four quadrants to help localise and diagnose symptoms or conditions more precisely. The quadrants are created by drawing a vertical line down the midline of the body and a horizontal line through the umbilicus. The four quadrants are:
- Right Upper Quadrant (RUQ)
- Left Upper Quadrant (LUQ)
- Right Lower Quadrant (RLQ)
- Left Lower Quadrant (LLQ)
1. Patient History
- Chief Complaint: Obtain a detailed description of the patient’s abdominal pain or discomfort, including location, intensity, duration, and any factors that relieve or exacerbate it. Ask if the pain is related to meals, bowel movements, or specific activities.
- Past Medical History: Investigate any previous gastrointestinal diseases, surgeries, or chronic conditions such as irritable bowel syndrome, Crohn’s disease, or peptic ulcer disease.
- Medications: Document all current medications, noting any that could cause gastrointestinal symptoms, such as NSAIDs, antibiotics, or laxatives.
- Dietary Habits: Assess the patient’s diet, focusing on recent changes in appetite or weight.
- Bowel and Bladder Function: Enquire about the frequency, consistency, and any changes in bowel movements and urination.
2. Inspection
This involves visually examining the abdomen for any abnormalities in size, shape, symmetry, skin condition, or movement with respiration.
- General Appearance: Observe the patient for signs of distress or discomfort.
- Skin: Check for colour changes, scars, striae (stretch marks), rashes, or lesions on the abdomen. Jaundice (yellowing of the skin and eyes), spider angiomas (small, red, spider-like veins on the skin) are dilated blood vessels visible on the skin’s surface. These can be associated with liver disease and cirrhosis,

- Contour and Symmetry: Note the shape of the abdomen (flat, rounded, distended) and check for symmetry.
- Visible Peristalsis: Look for visible movements of the intestines through the abdominal wall, which may indicate obstruction.
3. Auscultation
- Bowel Sounds: Listen for bowel sounds in all four quadrants using a stethoscope. Normal sounds are high-pitched and gurgling.
- Hypoactive: Reduced bowel sounds may indicate ileus or obstruction.
- Hyperactive: Increased bowel sounds may suggest diarrhoea or early obstruction.
- Absent: Lack of bowel sounds could indicate a severe obstruction or paralytic ileus.
- Bruits: Listen for vascular sounds over the aorta, renal arteries, iliac arteries, and femoral arteries. Bruits may indicate arterial stenosis.
4. Percussion
- General Percussion: This involves gently tapping the abdomen with the fingertips to assess the underlying organs. The sound produced can indicate the presence of fluid, gas, or masses.
- Tympany: A drum-like sound, indicating gas in the intestines.
- Dullness: A thud-like sound, which may indicate fluid (ascites) or a solid mass.
- Liver Span: Percuss the right midclavicular line to estimate the size of the liver.
- Splenic Percussion: Percuss the left upper quadrant to assess the size of the spleen.
5. Palpation
This involves feeling the abdomen with the hands to assess the size, consistency, and tenderness of the organs. The examiner will also feel for masses or hernias.
- Light Palpation: Gently press on the abdominal wall to assess for tenderness, masses, or rigidity.
- Tenderness: Note any areas of discomfort.
- Guarding: Involuntary tensing of the abdominal muscles, indicating peritonitis.
- Deep Palpation: Apply deeper pressure to feel for masses, organ enlargement, or deep tenderness.
- Rebound Tenderness: Press down slowly and then release quickly. Pain upon release may indicate peritonitis (Blumberg’s sign).
6. Special Tests
- Murphy’s Sign: Ask the patient to inhale while you press under the right costal margin. Pain upon inhalation may indicate cholecystitis.
- McBurney’s Point: Located one-third the distance from the anterior superior iliac spine to the umbilicus on the right side. Tenderness here suggests appendicitis.
- Rovsing’s Sign: Press deeply in the left lower quadrant and observe if pain is felt in the right lower quadrant, indicating appendicitis.
- Psoas Sign: Ask the patient to lift their right leg against resistance. Pain may indicate appendicitis or psoas abscess.
- Obturator Sign: Flex the patient’s right hip and knee, then rotate the leg internally and externally. Pain may indicate appendicitis.
Signs and Symptoms Being Observed For
- Pain: Location, intensity, and character of the pain.
- Tenderness: Specific areas of the abdomen that are tender to touch.
- Distention: Overall swelling of the abdomen.
- Nausea and Vomiting: Frequency and content of vomiting.
- Bowel Habits: Changes in frequency, consistency, and colour of stools.
- Urinary Symptoms: Changes in frequency, urgency, or pain during urination.
- Appetite Changes: Loss of appetite or unusual hunger.
- Weight Changes: Unexplained weight loss or gain.
- Jaundice: Yellowing of the skin or eyes, indicating liver dysfunction.
- Ascites: Accumulation of fluid in the abdomen, leading to swelling.
- Hernias: Protrusions of organs through the abdominal wall.
