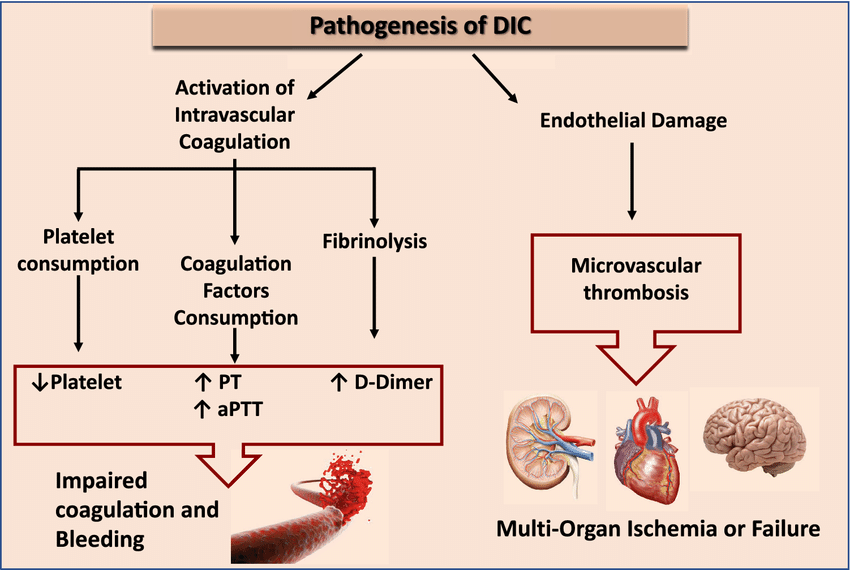
Disseminated intravascular coagulation (DIC), also known as consumptive coagulopathy, is a serious blood clotting disorder. It occurs when the body’s normal clotting mechanisms go awry, leading to widespread clotting throughout the small blood vessels (microvascular) in the body.
What happens in DIC
- Normally, blood clotting is a controlled process that helps prevent excessive bleeding after an injury.
- In DIC, however, the clotting process becomes activated abnormally. This can be triggered by various underlying conditions.
- The widespread activation of clotting factors leads to the formation of small blood clots throughout the body’s small vessels.
- As these microclots form, they use up clotting factors and platelets (cells involved in clotting) faster than they can be replaced.
- This depletion of clotting factors and platelets paradoxically leads to an increased risk of bleeding, even though the blood is clotting excessively
Pathophysiology
- Pathogen Interaction: In severe infections, especially bacterial sepsis, the body’s immune response is activated to combat the pathogen. This immune response includes the release of inflammatory cytokines such as tumour necrosis factor (TNF) and interleukins (IL-1, IL-6).
- Endothelial Damage: These cytokines cause damage to the endothelial lining of blood vessels, exposing the underlying tissue factor (TF), which is a potent initiator of the coagulation cascade.
- Release of Procoagulant Substances: Pathogens and damaged endothelial cells release substances that further activate the clotting system, leading to widespread clot formation.
DIC involves two main phases:
Stage 1: The thrombotic phase Stage
- Clot Formation: The coagulation system is abnormally activated, leading to the formation of blood clots in the small blood vessels throughout the body.
- Consumption of Clotting Factors: This excessive clotting uses up the body’s platelets and clotting factors, depleting their availability for normal clotting processes.
- Blood clots form and block small blood vessels, which can reduce or stop blood flow to organs and potentially damage them.
Stage 2: The bleeding phase
- Bleeding: Due to the depletion of clotting factors and platelets, the body cannot form clots effectively, leading to widespread bleeding.
Causes
DIC can be triggered by various underlying conditions, including:
- Sepsis: Severe infections, especially bacterial infections, can trigger the widespread activation of the clotting cascade.
- Severe Trauma: Major injuries, such as burns or head trauma, can lead to DIC.
- Malignancies: Certain cancers, particularly acute promyelocytic leukaemia and other solid tumours, are associated with DIC.
- Obstetric Complications: Conditions such as placental abruption, amniotic fluid embolism, and severe pre-eclampsia can trigger DIC.
- Severe Allergic Reactions: Anaphylaxis can lead to the activation of the coagulation system.
- Liver Disease: Advanced liver disease can predispose individuals to DIC due to impaired synthesis of clotting factors.
- Snakebites: Venom from some snakebites can activate clotting and cause DIC.Severe autoimmune reactions: Conditions like systemic lupus erythematosus (SLE) can sometimes cause DIC.
Clinical Presentation
The symptoms of DIC can vary widely depending on the underlying cause and the severity of the condition. Common signs and symptoms include:
- Bleeding: Such as petechiae (small red or purple spots), purpura (larger purple areas), ecchymoses (bruises), oozing from venipuncture sites, gastrointestinal bleeding, and haematuria (blood in the urine).
- Thrombosis: Symptoms related to thrombosis can include organ dysfunction (e.g., renal failure, respiratory distress, liver dysfunction) due to ischaemia.
- Shock: In severe cases, patients may present with signs of shock, including hypotension and tachycardia.
Diagnosis
Diagnosing DIC involves a combination of clinical assessment and laboratory tests:
- Clinical Assessment: Identifying the underlying cause and observing for signs of bleeding and thrombosis.
- Laboratory Tests:
- Prolonged prothrombin time (PT) and activated partial thromboplastin time (aPTT).
- Low platelet count.
- Elevated D-dimer levels.
- Reduced levels of fibrinogen.
- Elevated levels of fibrin degradation products (FDPs).
Treatment
The treatment of DIC focuses on addressing the underlying cause and managing the symptoms of bleeding and thrombosis:
- Treat the Underlying Cause: Effective management of the condition that triggered DIC (e.g., antibiotics for sepsis, surgery for trauma) is crucial.
- Supportive Care:
- Blood product replacement (e.g., platelets, fresh frozen plasma, cryoprecipitate) to manage bleeding.
- Anticoagulants (e.g., heparin) may be used cautiously in certain cases to control thrombosis, but this is controversial and depends on the clinical scenario.
- Close Monitoring: Regular monitoring of coagulation status, platelet counts, and overall clinical condition.
