Understanding the distribution and dynamics of body fluids is critical for clinical practice, particularly in managing fluid and electrolyte imbalances. This knowledge is essential in the UK healthcare setting, where guidelines and protocols are informed by organisations like NICE (National Institute for Health and Care Excellence).
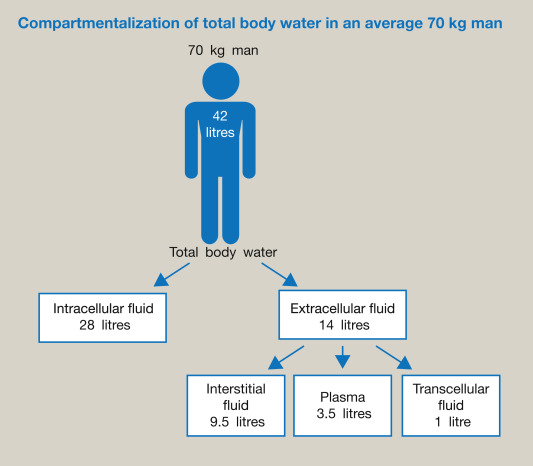
Intracellular Fluid (ICF): Accounts for about 60% of total body water. Extracellular Fluid (ECF): Accounts for about 40% of total body water.
1. Intracellular Fluid (ICF)
Description:
- Location: Fluid within the cells.
- Percentage of Total Body Water: Approximately 60%.
- Volume: About 25-30 liters in an average adult
- Key Components: High in potassium (K+), phosphate (PO4^3-), and magnesium (Mg^2+).
Clinical Relevance:
- Cellular Function: Maintains cellular structure and function, crucial for metabolic processes.
- Example: In cases of hyperkalemia, potassium primarily affects the ICF, necessitating interventions to shift potassium back into the cells (e.g., insulin-glucose therapy).
Example:
- Case: A patient with diabetic ketoacidosis (DKA) often presents with severe dehydration and electrolyte imbalances, requiring careful management of both ICF and ECF to restore cellular function and overall fluid balance.
2. Extracellular Fluid (ECF)
Description:
- Location: Fluid outside the cells.
- Percentage of Total Body Water: Approximately 40%.
- Volume: About 15-20 liters in an average adult.
- Subcompartments: Includes interstitial fluid, plasma, and transcellular fluid.
- Interstitial Fluid: Fluid between cells, making up about 75% of the ECF.
- About 10-15 liters.
- Plasma: The liquid component of blood, constituting about 25% of the ECF.
- Volume: About 3-5 liters.
- Transcellular Fluid: Includes cerebrospinal fluid, pleural fluid, peritoneal fluid, and others.
- Volume: About 1 liter.
Key Components:
- High in Sodium (Na+), Chloride (Cl-), and Bicarbonate (HCO3-).
Clinical Relevance:
- Volume and Pressure Regulation: Essential for maintaining blood pressure and volume.
- Example: In hypovolemic shock, rapid ECF restoration with isotonic crystalloids (e.g., 0.9% NaCl) is crucial to maintain blood pressure and perfusion.
Example:
- Case: A trauma patient with hemorrhagic shock needs immediate fluid resuscitation with crystalloids or colloids to restore plasma volume and ensure adequate tissue perfusion.
3. Transcellular Fluid
Description:
- Location: Specialised fluids such as cerebrospinal fluid, pleural fluid, peritoneal fluid, synovial fluid, and others.
- Percentage of Total Body Water: Small fraction, but significant in certain pathological conditions.
Clinical Relevance:
- Specialised Functions: Plays roles in lubrication, nutrient transport, and waste removal.
- Example: In conditions like ascites, excess fluid in the peritoneal cavity requires careful management, often involving paracentesis and diuretics.
Example:
- Case: A patient with liver cirrhosis and significant ascites may require therapeutic paracentesis to remove excess transcellular fluid and improve breathing and comfort.
Distribution of Body Water
- Total Body Water (TBW):
- Represents approximately 60% of body weight in adult males and 50-55% in adult females.
- Varies with age, sex, and body composition (higher in lean individuals and lower in obese individuals).
References and Guidelines
- NICE Guidelines:
- Intravenous Fluid Therapy in Adults in Hospital (CG174): Provides detailed recommendations for IV fluid therapy, including assessment of fluid needs, monitoring, and managing complications. NICE Guideline CG174.
- Royal College of Physicians (RCP):
- National Early Warning Score (NEWS) 2: A tool used to assess and respond to acute illness, including fluid balance assessment. RCP NEWS2.
- British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients (GIFTASUP):
- Provides evidence-based recommendations for fluid management in surgical patients, emphasising individualised assessment and monitoring.
Summary
Understanding fluid compartments and the principles of osmosis and diffusion is crucial for managing fluid therapy in ICU patients. Each compartment plays a distinct role in maintaining homeostasis, and interventions must be tailored to address specific imbalances. Adhering to UK guidelines ensures standardized and effective patient care, particularly in the dynamic and complex environment of the ICU.
