A GI bleed, refers to internal bleeding anywhere along the digestive tract, which includes the oesophagus (food pipe), stomach, small intestine, large intestine (colon), and rectum. This bleeding can be either mild or severe, and its location and severity determine the symptoms and treatment approach.
Classification:
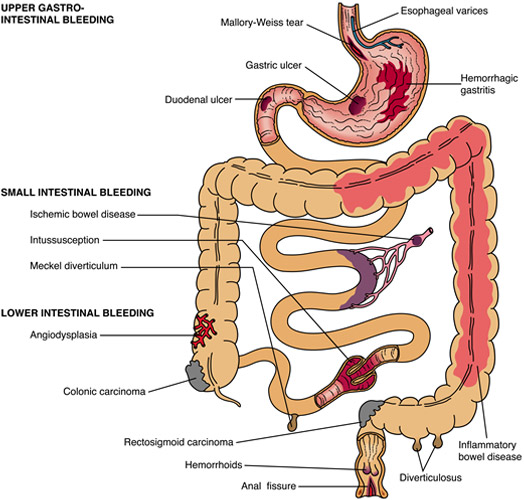
- Upper GI Bleed:
- Originates from the oesophagus, stomach, or duodenum.
- Common causes include peptic ulcers, oesophageal varices, gastritis, and Mallory-Weiss tears.
- Lower GI Bleed:
- Originates from the small intestine, colon, rectum, or anus.
- Common causes include diverticulosis, colorectal cancer, inflammatory bowel disease, haemorrhoids, and anal fissures.
Causes:
Upper GI Bleed:
- Peptic Ulcers: The most common cause, often associated with Helicobacter pylori infection or NSAID use.
- Oesophageal Varices: Enlarged veins in the oesophagus, commonly due to chronic liver disease and portal hypertension.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These medications, such as aspirin and ibuprofen, can irritate the stomach lining and increase the risk of ulcers and bleeding, especially with long-term use.
- Gastritis: Inflammation of the stomach lining, which can be caused by alcohol, NSAIDs, or infection.
- Mallory-Weiss Tear: A tear in the mucous membrane of the lower part of the oesophagus, often due to severe vomiting.
- Oesophagitis: Inflammation of the oesophagus, frequently related to gastro-oesophageal reflux disease (GORD).
Lower GI Bleed:
- Diverticulosis: Outpouchings of the colon wall that can bleed.
- Colorectal Cancer: Tumours in the colon or rectum can cause bleeding.
- Inflammatory Bowel Disease: Conditions like Crohn’s disease and ulcerative colitis.
- Haemorrhoids: Swollen veins in the lower rectum or anus.
- Anal Fissures: Small tears in the lining of the anus.
Symptoms:
Upper GI Bleed:
- Haematemesis: Vomiting blood, which may appear bright red or have a coffee-ground appearance.
- Melaena: Black, tarry stools due to the digestion of blood in the gastrointestinal tract.
- Epigastric Pain: Pain in the upper abdomen.
- Fatigue and Weakness: Due to blood loss and resulting anaemia.
Lower GI Bleed:
- Haematochezia: (Rectal Bleeding) Passage of bright red or maroon blood per rectum, often mixed with stool.
- Abdominal Pain: Cramping or discomfort.
- Fatigue and Weakness: As a result of chronic blood loss and anaemia.
Diagnosis:
- Clinical Assessment:
- History and Physical Examination: Assessing the patient’s symptoms, medical history, and performing a physical examination.
- Laboratory Tests:
- Complete Blood Count (CBC): To check for anaemia and the severity of blood loss.
- Coagulation Profile: To assess blood clotting function.
- Liver Function Tests: Particularly if liver disease is suspected.
- Imaging Studies:
- Endoscopy: The primary diagnostic tool for upper GI bleeding, allowing direct visualisation and potential therapeutic intervention.
- Colonoscopy: The primary diagnostic tool for lower GI bleeding, used to visualise the colon and rectum.
- CT Angiography: Can be useful in localising the source of active bleeding in cases where endoscopy is inconclusive.
- Radionuclide Scanning: Another method to locate active bleeding, particularly useful in obscure GI bleeding.
Management:
Initial Stabilisation:
- Resuscitation:
- IV Fluids: To maintain blood pressure and hydration.
- Blood Transfusion: For significant blood loss or anaemia.
- Monitoring:
- Vital Signs: Continuous monitoring of heart rate, blood pressure, and oxygen saturation.
- Urine Output: To assess kidney function and perfusion.
Specific Treatments:
Upper GI Bleed:
- Endoscopic Therapy:
- Injection Therapy: Using epinephrine to constrict blood vessels.
- Thermal Coagulation: Using heat to cauterise the bleeding vessel.
- Mechanical Methods: Such as clipping the bleeding vessel.
- Medications:
- Proton Pump Inhibitors (PPIs): To reduce stomach acid and stabilise clot formation.
- Example: High-dose intravenous omeprazole or esomeprazole.
- Antibiotics: In cases of suspected infection or in patients with oesophageal varices.
- Example: Ceftriaxone or quinolones for patients with cirrhosis to prevent bacterial infections.
- Proton Pump Inhibitors (PPIs): To reduce stomach acid and stabilise clot formation.
- Treatment of Variceal Bleeding:
- Vasoactive Drugs: Such as octreotide or terlipressin to reduce portal pressure.
- Band Ligation: Endoscopic procedure to place bands around the varices to stop bleeding.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS): A procedure to create a pathway between the portal and systemic circulation to reduce portal hypertension.
- Surgery:
- Reserved for cases where endoscopic treatment fails or in patients with ongoing bleeding.
Lower GI Bleed:
- Endoscopic Therapy:
- Polypectomy: Removal of polyps.
- Haemostasis: Using techniques similar to those for upper GI bleeding.
- Medications:
- Anti-inflammatory Drugs: For inflammatory bowel disease.
- Example: Mesalazine for ulcerative colitis or corticosteroids for acute flares.
- Topical Treatments: For haemorrhoids or anal fissures.
- Example: Topical nitroglycerin or diltiazem for anal fissures.
- Anti-inflammatory Drugs: For inflammatory bowel disease.
- Angiographic Interventions:
- Embolisation: Using angiography to locate and block the bleeding vessel.
- Surgery:
- May be necessary for diverticulosis with recurrent bleeding, colorectal cancer, or other structural causes.
- Segmental Resection: Removal of the affected part of the bowel.
- Total Colectomy: In cases of severe colitis or multiple bleeding sites.
Prognosis:
The prognosis of GI bleeding depends on the cause, severity, and promptness of treatment. Early detection and management are crucial for improving outcomes. Recurrent bleeding is a concern and may require long-term medical or surgical intervention.
