Altered Physiology in Relation to Hypertension
Hypertension, or high blood pressure, results from complex interactions between genetic, environmental, and physiological factors. Here’s an overview of the altered physiology that contributes to and results from hypertension:
1. Vascular Resistance
- Increased Peripheral Resistance: Hypertension often results from increased resistance in the small arteries (arterioles). This can be due to:
- Structural Changes: Thickening of the arterial walls (arteriolosclerosis), reducing lumen diameter.
- Functional Changes: Increased vascular tone due to enhanced vasoconstrictor activity (e.g., increased sympathetic nervous system activity).
2. Cardiac Output
- Increased Blood Volume: Retention of sodium and water by the kidneys increases blood volume, raising cardiac output and blood pressure.
- Increased Heart Rate and Contractility: Elevated sympathetic nervous system activity can increase heart rate and myocardial contractility, contributing to higher cardiac output.
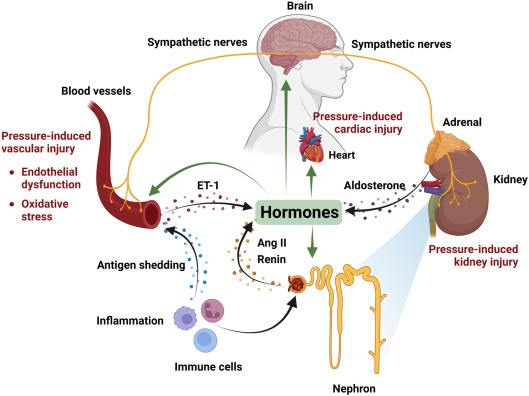
3. Renin-Angiotensin-Aldosterone System (RAAS)
- Activation of RAAS: Hypertension can be driven by overactivity of the RAAS. Key components include:
- Renin Release: Stimulated by decreased renal perfusion or sympathetic activation, leading to increased angiotensin II production.
- Angiotensin II: Causes vasoconstriction, increased aldosterone secretion (promoting sodium and water retention), and sympathetic nervous system activation.
- Aldosterone: Increases sodium and water reabsorption in the kidneys, contributing to increased blood volume.
4. Endothelial Dysfunction
- Reduced Nitric Oxide (NO) Production: NO is a vasodilator produced by the endothelium. Reduced NO levels lead to increased vascular tone and resistance.
- Increased Endothelin: Endothelin is a potent vasoconstrictor. Elevated levels contribute to increased vascular resistance.
5. Sympathetic Nervous System
- Increased Sympathetic Activity: Chronic stress, obesity, and other factors can lead to overactivity of the sympathetic nervous system, causing increased heart rate, contractility, and vasoconstriction.
6. Genetic and Environmental Factors
- Genetic Predisposition: Certain genetic variations can predispose individuals to hypertension by affecting sodium handling, vascular tone, or hormonal regulation.
- Environmental Factors: Lifestyle factors such as high salt intake, obesity, lack of physical activity, and excessive alcohol consumption can contribute to the development and exacerbation of hypertension.
7. Kidney Function
- Impaired Natriuresis: The kidneys’ ability to excrete sodium may be impaired, leading to sodium retention, increased blood volume, and hypertension.
- Renal Artery Stenosis: Narrowing of the arteries supplying the kidneys can lead to increased renin release and secondary hypertension.
8. Hormonal Influences
- Adrenal Gland Disorders: Conditions such as hyperaldosteronism (Conn’s syndrome) and pheochromocytoma can cause excessive hormone production leading to hypertension.
- Insulin Resistance: Common in metabolic syndrome and diabetes, insulin resistance can lead to endothelial dysfunction, increased sympathetic activity, and altered sodium handling, contributing to hypertension.
9. Baroreceptors and Hypertension
- Baroreceptors in the Aorta and Carotid Arteries:
- Location and Function: Baroreceptors are stretch-sensitive mechanoreceptors located primarily in the aortic arch and carotid sinuses. They detect changes in blood pressure by sensing the stretch of the arterial walls.
- Normal Response: When blood pressure increases, baroreceptors are activated and send signals to the brainstem (medulla oblongata), which in turn activates the parasympathetic nervous system and inhibits the sympathetic nervous system. This leads to decreased heart rate, vasodilation, and reduced cardiac output and peripheral resistance, ultimately lowering blood pressure.
- Hypertension Implications: In chronic hypertension, baroreceptors can become desensitized or reset to a higher baseline pressure, making them less effective at regulating elevated blood pressure. This impaired baroreceptor sensitivity means that the body does not respond appropriately to high blood pressure, perpetuating hypertension.
- Adrenal Glands and Hypertension:
- Hormone Secretion: The adrenal glands produce hormones such as aldosterone, adrenaline (epinephrine), and norepinephrine, which play crucial roles in blood pressure regulation.
- Aldosterone: Regulates sodium and water balance. Excessive aldosterone secretion (e.g., in primary hyperaldosteronism) leads to sodium and water retention, increasing blood volume and blood pressure.
- Adrenaline and Norepinephrine: These catecholamines increase heart rate, contractility, and vasoconstriction, raising blood pressure.
Summary
- Increased Peripheral Resistance: Due to structural and functional changes in small arteries.
- Increased Blood Volume: Resulting from sodium and water retention.
- RAAS Activation: Leading to vasoconstriction, increased blood volume, and sympathetic activation.
- Endothelial Dysfunction: Decreased NO production and increased endothelin levels.
- Sympathetic Overactivity: Causing increased heart rate, contractility, and vasoconstriction.
- Genetic and Environmental Factors: Including dietary habits, obesity, and lifestyle choices.
- Impaired Kidney Function: Affecting sodium excretion and blood volume regulation.
- Hormonal Influences: From adrenal gland disorders and insulin resistance.
- Baroreceptor Desensitisation: Chronic hypertension leads to less effective baroreceptor signaling, allowing high blood pressure to persist.
- Hormonal Imbalance: Conditions like hyperaldosteronism and pheochromocytoma increase blood pressure through excessive hormone production affecting blood volume and vascular tone.
Understanding these physiological alterations is crucial for developing effective treatment strategies to manage and mitigate hypertension and its associated risks.
