Inotropes are drugs that influence the strength of heart muscle contractions. They are primarily used in the management of heart failure, certain types of shock, and other cardiovascular conditions.
Types of Inotropes
Inotropes are classified into two main categories: positive inotropes, which increase the force of heart contractions, and negative inotropes, which decrease it.
Positive Inotropes
- Catecholamines
- Adrenaline (Epinephrine)
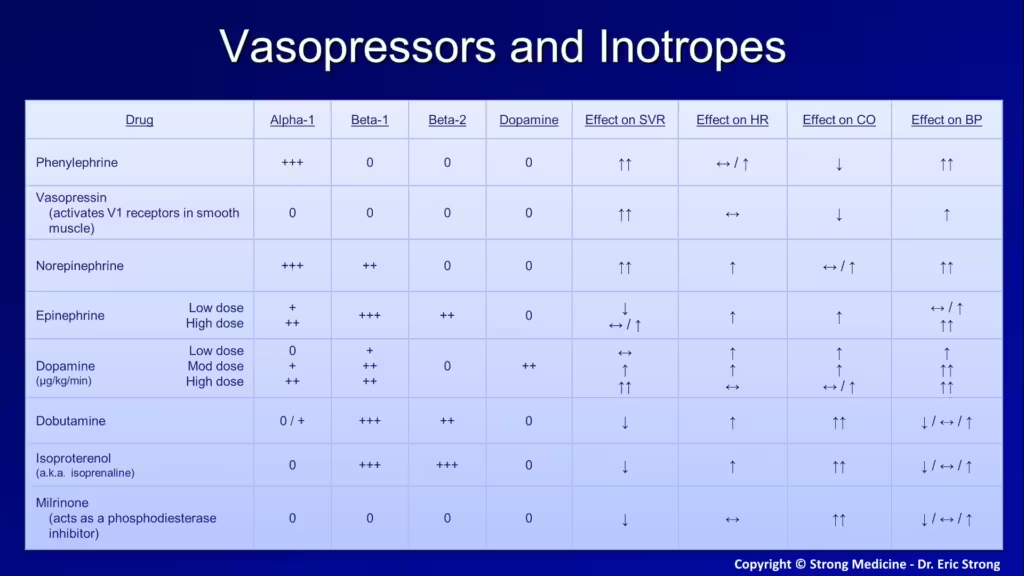
- Mechanism: Acts on alpha and beta-adrenergic receptors to increase heart rate and contractility.
- Uses: Cardiac arrest, anaphylaxis, severe asthma attacks.
- Dose: 1 mg IV push for cardiac arrest, repeated every 3-5 minutes; 0.3-0.5 mg intramuscular for anaphylaxis.
- Adverse Effects: Tachycardia, hypertension, arrhythmias, anxiety, palpitations.
- Contraindications: None in emergency settings, caution in patients with hypertension or ischemic heart disease.
- Noradrenaline (Norepinephrine)
- Mechanism: Primarily stimulates alpha-adrenergic receptors, causing vasoconstriction and modestly increasing cardiac output.
- Uses: Septic shock, severe hypotension.
- Dose: 0.1-0.5 mcg/kg/min IV infusion, titrated to effect.
- Adverse Effects: Hypertension, arrhythmias, peripheral ischemia.
- Contraindications: Mesenteric or peripheral vascular thrombosis, pregnancy.
- Dopamine
- Mechanism: Dose-dependent effects; low doses increase renal perfusion, moderate doses increase heart rate and contractility, high doses cause vasoconstriction.
- Uses: Heart failure, shock.
- Dose: 2-20 mcg/kg/min IV infusion.
- Adverse Effects: Tachycardia, arrhythmias, nausea, tissue necrosis with extravasation.
- Contraindications: Pheochromocytoma, uncorrected tachyarrhythmias, ventricular fibrillation.
- Dobutamine
- Mechanism: Selectively stimulates beta-1 adrenergic receptors, increasing heart rate and contractility with less effect on peripheral vascular resistance.
- Uses: Acute heart failure, cardiogenic shock.
- Dose: 2-20 mcg/kg/min IV infusion.
- Adverse Effects: Tachycardia, arrhythmias, hypotension.
- Contraindications: Idiopathic hypertrophic subaortic stenosis, uncorrected hypovolemia.
- Adrenaline (Epinephrine)
- Phosphodiesterase Inhibitors
- Milrinone
- Mechanism: Inhibits phosphodiesterase-3, leading to increased cAMP levels and enhanced myocardial contractility.
- Uses: Acute heart failure, severe exacerbations of chronic heart failure.
- Dose: 0.125-0.75 mcg/kg/min IV infusion.
- Adverse Effects: Hypotension, arrhythmias, thrombocytopenia.
- Contraindications: Severe aortic or pulmonic valvular disease, acute myocardial infarction.
- Levosimendan
- Type: Calcium sensitizer and phosphodiesterase-3 inhibitor
- Dose: Loading dose: 12 µg/kg over 10 min; maintenance: 0.1-0.2 µg/kg/min
- Half-life: 1 hour (active metabolite 75-80 hours)
- Bioavailability: Administered intravenously, 100% bioavailability
- Indications: Acute decompensated heart failure
- Side Effects: Hypotension, headache, arrhythmias
- Milrinone
- Cardiac Glycosides
- Digoxin
- Mechanism: Inhibits Na+/K+ ATPase, increasing intracellular calcium and enhancing cardiac contractility.
- Uses: Chronic heart failure, atrial fibrillation.
- Dose: Loading dose of 0.5-1 mg IV or PO, maintenance dose of 0.125-0.5 mg daily.
- Adverse Effects: Bradycardia, nausea, vomiting, visual disturbances, arrhythmias.
- Contraindications: Ventricular fibrillation, digoxin hypersensitivity, caution in patients with renal impairment.
- The sodium-potassium pump (Na⁺/K⁺-ATPase) is an essential membrane protein that maintains the electrochemical gradient across the cell membrane. It works as follows:
- Sodium Movement: The pump exports three sodium ions (Na⁺) out of the cell.
- Potassium Movement: The pump imports two potassium ions (K⁺) into the cell.
- This process consumes one molecule of ATP, which provides the energy needed to move these ions against their respective concentration gradients. The pump is crucial for maintaining the resting membrane potential and is vital for nerve impulse transmission and muscle contraction.
- The sodium-calcium exchanger (NCX) is a membrane protein that plays a crucial role in maintaining cellular calcium balance, especially in cardiac cells. It operates by exchanging three sodium ions (Na⁺) for one calcium ion (Ca²⁺) across the cell membrane, typically moving calcium out of the cell while allowing sodium to enter. This exchanger is vital for cardiac muscle relaxation following contraction and is tightly linked to the function of the sodium-potassium ATPase pump. The NCX helps regulate intracellular calcium levels, which are essential for proper heart muscle contraction and relaxation.
- Directionality: Normally exports Ca²⁺ from the cell and imports Na⁺.
- Role in Digoxin Action: When Na⁺/K⁺-ATPase is inhibited (e.g., by digoxin), increased intracellular Na⁺ reduces NCX activity, leading to higher intracellular Ca²⁺ levels, which enhances cardiac contractility.
- Digoxin
Negative Inotropes
- Beta-Blockers
- Mechanism: Block beta-adrenergic receptors, reducing heart rate and contractility.
- Uses: Hypertension, chronic heart failure, arrhythmias.
- Examples: Metoprolol, propranolol, carvedilol.
- Adverse Effects: Bradycardia, hypotension, fatigue, bronchospasm.
- Contraindications: Asthma, severe bradycardia, heart block, cardiogenic shock.
- Calcium Channel Blockers
- Mechanism: Inhibit calcium entry into cardiac cells, reducing contractility.
- Uses: Hypertension, angina, certain arrhythmias.
- Examples: Verapamil, diltiazem.
- Adverse Effects: Bradycardia, hypotension, peripheral edema, constipation.
- Contraindications: Severe hypotension, cardiogenic shock, severe left ventricular dysfunction.
