Abdominal hypertension, also known as intra-abdominal hypertension (IAH), is a condition characterised by elevated pressure within the abdominal cavity. It can lead to significant morbidity and mortality due to its impact on abdominal organs and systemic circulation.
- Normal: Less than 5 mmHg
- IAH: Greater than or equal to 12 mmHg (persistent)
Categories of IAH :
- Grade I: IAP 12-15 mmHg (Mild)
- Grade II: IAP 16-20 mmHg (Moderate)
- Grade III: IAP 21-25 mmHg (Severe)
- Grade IV: IAP >25 mmHg (Very Severe)
Definition
- Intra-Abdominal Hypertension (IAH): A sustained or repeated pathological elevation of intra-abdominal pressure (IAP) equal to or greater than 12 mmHg.
- Abdominal Compartment Syndrome (ACS): A severe form of IAH where the intra-abdominal pressure exceeds 20 mmHg and is associated with new organ dysfunction or failure.
Causes
IAH can result from a variety of conditions that increase intra-abdominal volume or decrease abdominal wall compliance:
- Increased Intra-Abdominal Volume:
- Ascites: Accumulation of fluid in the abdominal cavity.
- Hemoperitoneum: Presence of blood in the peritoneal cavity.
- Massive fluid resuscitation: Large volumes of fluid administered intravenously, commonly seen in critical care settings.
- Bowel distension: Due to obstruction, ileus, or infection.
- Decreased Abdominal Wall Compliance:
- Obesity: Excess adipose tissue increases abdominal pressure.
- Abdominal trauma: Injury leading to swelling and bleeding within the abdominal cavity.
- Postoperative conditions: Abdominal surgery can reduce compliance due to pain, muscle dysfunction, or dressings.
Pathophysiology
Elevated intra-abdominal pressure can compress abdominal organs, impairing their function and leading to systemic effects:
- Organ Compression:
- Kidneys: Reduced renal perfusion leading to acute kidney injury.
- Liver: Impaired hepatic blood flow causing liver dysfunction.
- Gut: Decreased mesenteric blood flow leading to bowel ischemia and necrosis.
- Systemic Effects:
- Cardiovascular: Increased intra-thoracic pressure, reduced venous return, and cardiac output.
- Respiratory: Diaphragmatic elevation leading to reduced lung volumes and compliance, resulting in respiratory distress.
- Central Nervous System: Increased intracranial pressure due to impaired venous return from the brain.
Methods of Measuring Intra-Abdominal Pressure (IAP)
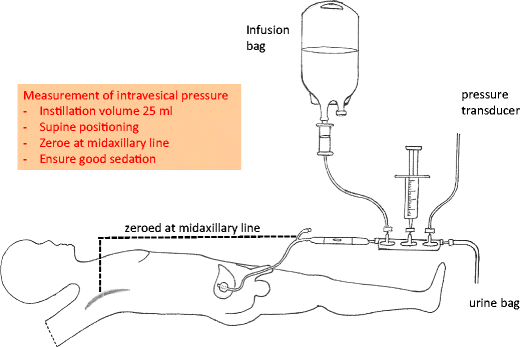
- Trans-Bladder (Intravesical) Pressure Measurement
- Procedure:
- A Foley catheter is inserted into the bladder.
- The bladder is partially filled with a sterile saline solution (typically 50-100 mL).
- A pressure transducer is connected to the catheter, and the patient is positioned supine.
- The pressure is measured at the end of expiration to avoid fluctuations due to respiratory movements.
- Advantages:
- Non-invasive and relatively simple to perform.
- Widely accepted as the standard method for IAP measurement.
- Considerations:
- Ensuring the bladder is not overfilled is critical, as this can affect accuracy.
- Procedure:
- Trans-Gastric Pressure Measurement
- Procedure:
- A nasogastric tube is placed into the stomach.
- The tube is connected to a pressure transducer.
- Measurements are taken similarly to the trans-bladder method, ensuring the patient is in a supine position and measurements are taken at end-expiration.
- Advantages:
- Useful in patients where bladder catheterisation is contraindicated.
- Considerations:
- Less commonly used than the trans-bladder method.
- May be less accurate due to potential complications with gastric contents.
- Procedure:
- Direct Intraperitoneal Pressure Measurement
- Procedure:
- Performed during surgery or via a percutaneous catheter placed directly into the abdominal cavity.
- A pressure transducer is attached directly to the catheter to measure the intra-abdominal pressure.
- Advantages:
- Provides a direct and highly accurate measurement of IAP.
- Considerations:
- Invasive and typically reserved for surgical settings.
- Procedure:
- Rectal Pressure Measurement
- Procedure:
- A rectal catheter is inserted, and a pressure transducer is used to measure IAP.
- Advantages:
- Another alternative when bladder or gastric measurements are not feasible.
- Considerations:
- Not widely used and may have varying accuracy depending on patient condition.
- Procedure:
Clinical Management
Management of IAH and ACS involves both medical and surgical approaches:
- Medical Management:
- Fluid Management: Careful regulation of intravenous fluids to avoid over-resuscitation.
- Diuretics: Used to reduce fluid accumulation.
- Paracentesis: Removal of excess abdominal fluid in cases of ascites.
- Surgical Management:
- Decompression Laparotomy: Emergency surgery to relieve pressure in severe cases.
- Abdominal Wall Reconstruction: For cases where decreased abdominal compliance is due to structural issues.
- Supportive Care:
- Optimising Ventilation: Mechanical ventilation adjustments to improve respiratory function.
- Monitoring and Support: Continuous monitoring of organ function and prompt treatment of organ failure.
