Inverse ratio ventilation (IRV) is a ventilation strategy used in mechanical ventilation to improve oxygenation in patients with respiratory problems. It works by altering the typical breathing pattern to prioritise inhalation over exhalation.
Here’s a breakdown of IRV:
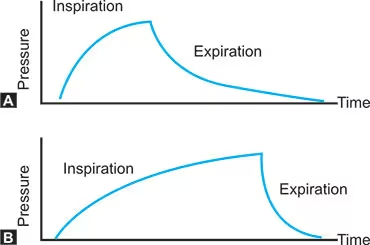
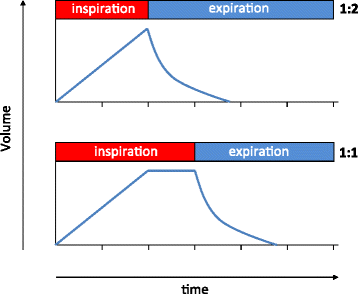
- Normal Ventilation: In normal breathing, the time spent inhaling (inspiration) is shorter than the time spent exhaling (expiration). This creates an inspiratory to expiratory (I:E) ratio of around 1:2.
- Inverse Ratio: IRV flips this ratio, extending the inspiratory phase and shortening the expiratory phase. Common I:E ratios used in IRV might be 2:1 or 3:1.
Normal Breath Cycle:
- Cycle Duration: 60 seconds / 10 breaths = 6 seconds per breath.
- Normal I:E Ratio: 1:2
- Inspiration: 2 seconds
- Expiration: 4 seconds
Inverse Ratio Ventilation (IRV):
- Cycle Duration: 6 seconds per breath
- IRV I:E Ratio: 2:1
- Inspiration: 4 seconds
- Expiration: 2 seconds
How IRV Works:
- Increased Mean Airway Pressure: By prolonging the inspiratory phase, IRV increases the mean airway pressure, which helps in keeping the alveoli open (alveolar recruitment) and improving oxygenation.
- Promotion of Alveolar Recruitment: Prolonged inspiratory time helps in maintaining alveolar patency, preventing collapse, and thus improving gas exchange.
- Improved Oxygenation: With more alveoli open for longer periods, oxygen uptake is increased, which is crucial for patients with severe respiratory failure like ARDS.
Indications:
- Severe Hypoxemia: Particularly in ARDS where conventional ventilation strategies fail to maintain adequate oxygenation.
- Refractory Hypoxemia: When patients do not respond to high levels of positive end-expiratory pressure (PEEP) or other ventilatory adjustments.
- Inverse Ratio Ventilation (IRV) can be beneficial in addressing shunting and ventilation/perfusion (V/Q) mismatch, which are common issues in severe respiratory conditions like ARDS.
- Shunting: Alveolar Recruitment: IRV increases the duration of alveolar inflation, helping to open collapsed alveoli, which reduces shunting (blood passing through the lungs without being oxygenated)
- V/Q Mismatch: Improved Oxygenation: By maintaining higher mean airway pressures and increasing the time alveoli remain open, IRV enhances oxygenation, improving the match between ventilation and perfusion in the lungs.
Settings and Monitoring:
- I:E Ratio: Adjusted based on the patient’s needs, starting from a 1:1 ratio or 2:1 potentially extending to 3:1 or higher.
- Tidal Volume: Typically set lower than in conventional ventilation to prevent volutrauma.
- PEEP: Carefully monitored to prevent air trapping and auto-PEEP, which can occur due to insufficient expiratory time.
Complications and Management:
- Auto-PEEP: Caused by insufficient expiratory time leading to air trapping, which can increase the risk of barotrauma and haemodynamic instability.
- Patient Discomfort: Extended inspiratory time can be uncomfortable, often necessitating sedation or neuromuscular blockade to ensure patient-ventilator synchrony.
- Hemodynamic Effects: Increased mean airway pressure can affect venous return and cardiac output, requiring careful haemodynamic monitoring and management.
Summery
IRV is used to treat a number of conditions, including: Acute respiratory distress syndrome (ARDS) in adults, Acute lung injury, and Hyaline membrane disease in neonates.
Some studies have shown that IRV can improve gas exchange over conventional ventilatory modes and prevent end-expiratory lung collapse. However, other studies have found that IRV doesn’t improve important clinical outcomes, such as mortality or duration of mechanical ventilation. This may be because IRV isn’t considered early enough once ARDS is diagnosed.
References:
- NCBI Bookshelf – Inverse Ratio Ventilation (IRV)
