Neurogenic shock is a type of distributive shock resulting from the loss of sympathetic nervous system signals to the blood vessels, causing widespread vasodilation, decreased systemic vascular resistance, and subsequent hypotension. This condition is often associated with severe spinal cord injuries at or above T6, but can also result from traumatic brain injuries or certain pharmacological agents. The T6 level is particularly critical because it is a key point for sympathetic outflow that controls the vascular tone of blood vessels.
Understanding the Mechanism:
Normally, the autonomic nervous system maintains a delicate balance between two branches:
- Sympathetic nervous system (SNS): Acts like an accelerator, increasing heart rate, blood pressure, and blood vessel constriction during times of stress or activity.
- Parasympathetic nervous system (PNS): Acts like a brake, promoting relaxation and slowing down heart rate and blood vessel constriction.
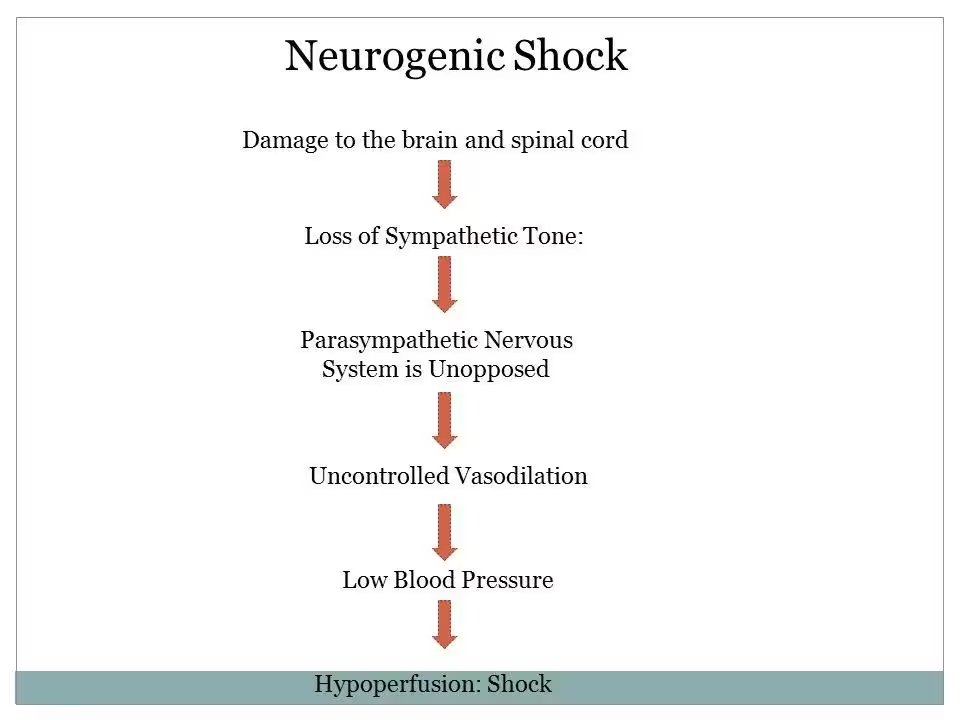
In neurogenic shock, something disrupts this balance. Here’s what happens:
Pathophysiology:
The pathophysiology of neurogenic shock involves several key mechanisms:
- Loss of Sympathetic Tone:
- Spinal Cord Injury: Damage to the spinal cord, particularly at or above the T6 level, disrupts sympathetic outflow.
- Brain Injury: Traumatic brain injuries can impair the autonomic nervous system control centers.
- Pharmacological Agents: Certain medications (e.g., anesthetics, sedatives) can inhibit sympathetic nervous system activity.
2. Vasodilation & Bradycardia
- Peripheral Vasodilation: The loss of sympathetic tone leads to unopposed parasympathetic activity, causing widespread vasodilation.
- Decreased Systemic Vascular Resistance: This reduction in vascular tone lowers systemic vascular resistance, leading to hypotension.
- Reduced Sympathetic Stimulation: The heart rate can decrease (bradycardia) due to the loss of sympathetic input and unopposed parasympathetic influence.
- The decrease in sympathetic tone causes the blood vessels in the lower extremities to dilate. This dilation reduces the amount of blood returning to the heart, leading to low blood pressure (hypotension) and shock. Additionally, the lack of sympathetic control over the heart allows unopposed vagal influence, resulting in a slow heart rate (bradycardia). (Dave, Dahlstrom, & Weisbrod, 2023)
4. Impaired Blood Flow:
- Inadequate Tissue Perfusion: The combination of hypotension and bradycardia results in reduced cardiac output and inadequate tissue perfusion, leading to hypoxia and potential organ dysfunction.
5. Secondary Injury:
Secondary spinal cord injury develops within hours to days after the initial trauma. This phase is caused by vascular disturbances, electrolyte imbalances, and the development of edema, leading to gradual central hemorrhagic necrosis within the gray matter at the injury site.
Identification:
Early recognition of neurogenic shock is critical for effective treatment. Identification involves clinical assessment and diagnostic testing:
- Clinical Symptoms:
- Hypotension (low blood pressure) despite adequate fluid resuscitation
- Bradycardia (slow heart rate)
- Warm, Pink & dry skin due to vasodilation (of subcutaneous blood vessels)
- Signs of spinal cord injury (e.g., loss of motor and sensory function below the level of injury)
- Altered mental status (confusion, lethargy)
2. Physical Examination:
- Assess for signs of spinal cord or brain injury
- Evaluate heart rate and blood pressure
- Check for signs of poor perfusion (e.g., delayed capillary refill, cyanosis)
3. Diagnostic Tests:
- Imaging Studies: MRI or CT scans to identify spinal cord injuries or brain injuries.
- Electrocardiogram (ECG): To monitor heart rate and rhythm.
- Haemodynamic Monitoring: To assess blood pressure and cardiac output.
- Laboratory Tests: To rule out other causes of shock and assess organ function.
Management:
Management of neurogenic shock focuses on stabilising the patient, restoring sympathetic tone, and providing supportive care to maintain organ function:
- Initial Stabilisation:
- Fluid Resuscitation: Administer isotonic crystalloids (e.g., normal saline or Plasmolyte) to maintain intravascular volume.
- Vasopressors: Use vasopressors (e.g., norepinephrine, phenylephrine) to counteract vasodilation and maintain blood pressure. (Norepinephrine is preferred due to its dual α- and β-activity, effectively addressing hypotension and bradycardia) (However, phenylephrine lacks β-activity, so it can cause reflex bradycardia) (Dave, Dahlstrom, & Weisbrod, 2023).
- Atropine: Administer atropine if significant bradycardia is present to increase heart rate.
- Pacing: In cases of severe bradycardia that do not respond to pharmacologic interventions, temporary transcutaneous or transvenous pacing may be necessary to maintain adequate heart rate and cardiac output.
2. Addressing Underlying Cause:
- Spinal Cord Injury: Immobilise the spine and consult neurosurgery for potential surgical intervention.
- Brain Injury: Manage intracranial pressure and consider surgical options if necessary.
3. Supportive Care:
- Oxygen Therapy: Ensure adequate oxygenation and, if necessary, provide mechanical ventilation.
- Monitoring: Continuous monitoring of vital signs, urine output, and laboratory parameters to assess response to treatment.
- Temperature Regulation: Maintain normothermia as patients with neurogenic shock may have impaired thermoregulation.
4. Long-term Management:
- Rehabilitation: Initiate physical and occupational therapy to support recovery and manage long-term disabilities.
- Medications: Use medications to manage symptoms and prevent complications.
- Follow-up: Regular follow-up with healthcare providers to monitor recovery and address any ongoing issues.
References:
