Definition:
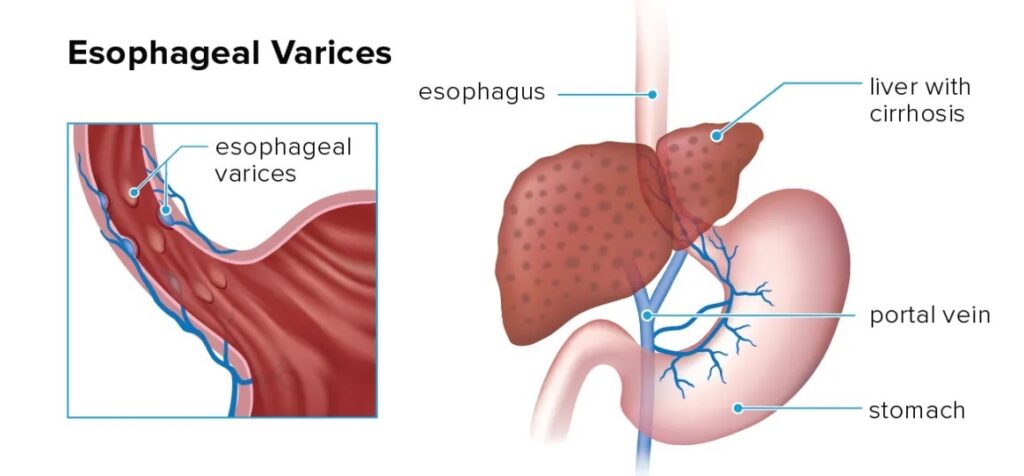
Oesophageal varices are enlarged veins in the lower part of the oesophagus. They develop due to increased pressure in the portal venous system, a condition known as portal hypertension. This increased pressure forces blood to flow through smaller veins that are not equipped to handle such volume, causing them to swell and potentially rupture, leading to life-threatening bleeding.
Understanding Portal Circulation:
Normal Portal Circulation:
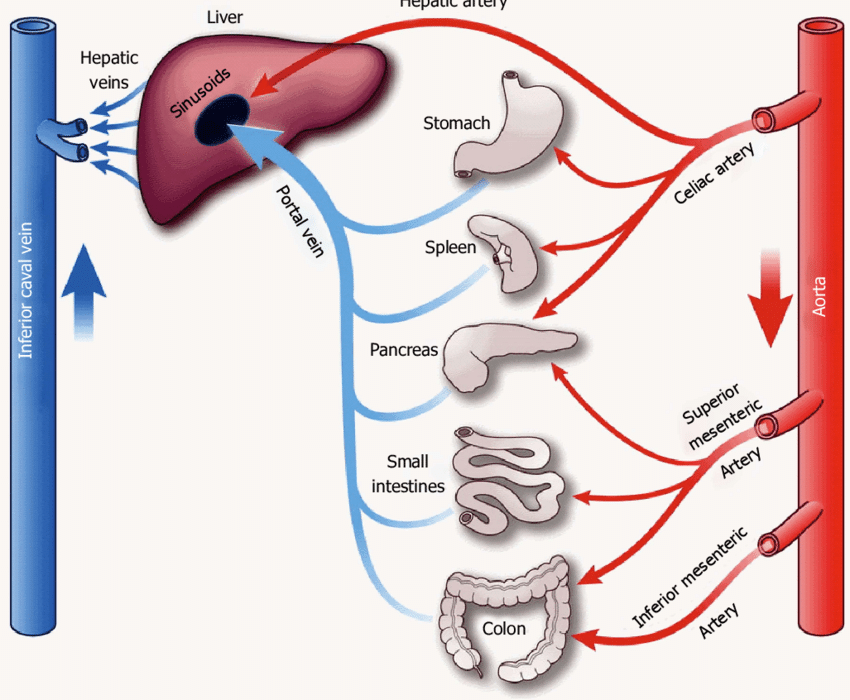
- The portal vein carries blood from the digestive organs (stomach, intestines, spleen, and pancreas) to the liver. This blood is rich in nutrients but also contains toxins and metabolic byproducts.
- In the liver, blood is filtered, detoxified, and then sent to the heart via the hepatic veins.
Portal Hypertension:
- Portal hypertension is an increase in the blood pressure within the portal venous system. This can be caused by liver diseases such as cirrhosis, which leads to scarring and obstruction of blood flow through the liver.
- When the liver is scarred, the blood flow is restricted, causing pressure to build up in the portal vein. This increased pressure forces blood to find alternative pathways through collateral veins, including those in the oesophagus, leading to the formation of varices.
Causes of Oesophageal Varices:
- Liver Cirrhosis:
- Cirrhosis is the most common cause of oesophageal varices. Chronic liver diseases like hepatitis B and C, alcohol-related liver disease, and non-alcoholic fatty liver disease can lead to cirrhosis.
- Portal Vein Thrombosis:
- Blood clots in the portal vein can obstruct blood flow, increasing pressure and leading to varices.
- Schistosomiasis:
- A parasitic infection that can cause liver damage and portal hypertension, particularly in tropical regions.
Symptoms of Oesophageal Varices:
- Bleeding: The most severe symptom, which can present as:
- Haematemesis: Vomiting blood, which can be bright red or have a coffee-ground appearance due to partial digestion of blood.
- Melaena: Black, tarry stools from digested blood.
- Haematochezia: Passage of bright red blood per rectum, indicating severe bleeding.
- Signs of Anaemia: Fatigue, pallor, and weakness due to blood loss.
- Shock: In cases of significant blood loss, symptoms can include low blood pressure, rapid heart rate, and confusion.
Diagnosis of Oesophageal Varices:
- Endoscopy:
- The gold standard for diagnosing oesophageal varices. An endoscope is inserted through the mouth to visually inspect the oesophagus for swollen veins.
- Imaging:
- Ultrasound (Doppler): Evaluates blood flow in the portal vein and can identify liver cirrhosis.
- CT Scan/MRI: Provides detailed images of the liver and surrounding blood vessels to assess for portal hypertension.
- Laboratory Tests:
- Liver Function Tests: Evaluate the extent of liver damage.
- Complete Blood Count (CBC): Detects anaemia and checks platelet levels.
- Coagulation Profile: Assesses blood clotting ability, which can be impaired in liver disease.
- Upper Gastrointestinal (GI) Series:
- This is a radiographic examination of the upper GI tract, including the oesophagus, stomach, and duodenum. It involves swallowing a barium solution that coats the lining of the upper GI tract, making it visible on X-rays. This test can help in identifying oesophageal varices by highlighting irregularities in the contour of the oesophagus.
Management of Oesophageal Varices:
Initial Stabilisation:
- Resuscitation:
- IV Fluids and Blood Transfusions: To stabilise blood pressure and replace lost blood.
- Vasoactive Drugs: Medications like octreotide or terlipressin to reduce portal pressure and slow bleeding.
- Monitoring:
- Vital Signs: Continuous monitoring to detect any signs of deterioration.
- Urine Output: To assess kidney function and ensure adequate perfusion.
Specific Treatments:
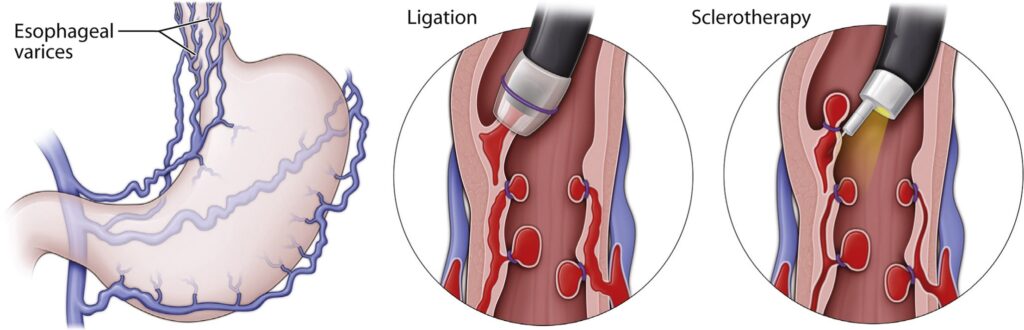
- Endoscopic Therapy:
- Band Ligation: Small bands are placed around the varices to cut off blood flow and cause the veins to shrink. This is the preferred method for treating bleeding varices.
- Sclerotherapy: Injection of a sclerosing agent into the varices to induce clotting and sclerosis, used when band ligation is not feasible. Some examples are (hypertonic saline, sodium tetradecyl sulfate, polidocanol, and chromated glycerin)
- Pharmacological Therapy:
- Beta-Blockers: Non-selective beta-blockers like propranolol or nadolol to reduce portal hypertension and prevent rebleeding.
- Antibiotics: Prophylactic antibiotics (e.g., ceftriaxone or norfloxacin) to prevent infections, which are common in patients with variceal bleeding.
- Balloon Tamponade:
- Sengstaken-Blakemore Tube: A temporary measure using a balloon catheter to control severe bleeding when endoscopic therapy is not immediately available.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS):
- A radiologic procedure to create a channel within the liver, connecting the portal vein to the hepatic vein, thereby reducing portal pressure.
- Surgery:
- Shunt Surgery: Creating an alternate pathway for blood flow to reduce portal pressure.
- Liver Transplantation: Considered for patients with end-stage liver disease who are not candidates for other treatments.
Complications of Oesophageal Varices:
- Rebleeding:
- There is a high risk of rebleeding, especially within the first few days to weeks after an initial bleed. Close monitoring and follow-up are essential.
- Infections:
- Increased risk of bacterial infections, particularly spontaneous bacterial peritonitis.
- Hepatic Encephalopathy:
- A decline in brain function due to the liver’s inability to remove toxins from the blood, exacerbated by the diversion of blood flow away from the liver.
Prognosis:
- The prognosis depends on the severity of liver disease and the effectiveness of the treatment. Early diagnosis and management significantly improve outcomes, but recurrent bleeding and liver failure remain concerns.
