Oesophagectomy: Detailed Overview
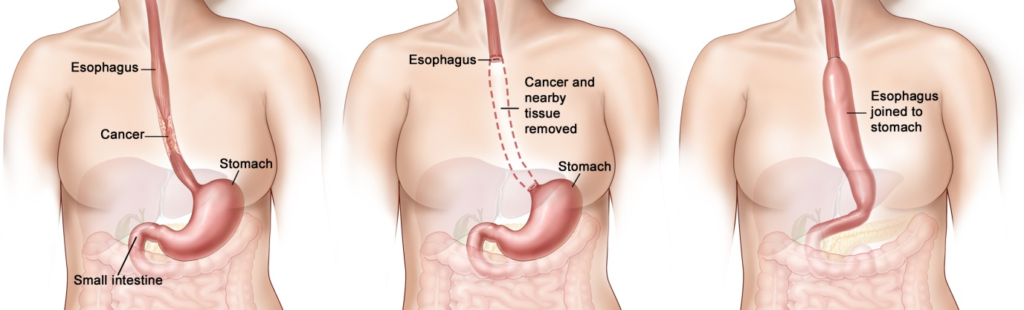
An oesophagectomy is a surgical procedure to remove part or all of the oesophagus, the tube that connects the throat to the stomach. This procedure is primarily used to treat oesophageal cancer, but it can also be indicated for other conditions such as Barrett’s oesophagus with high-grade dysplasia, severe oesophageal stricture, or oesophageal perforation.
Indications
Oesophagectomy is typically indicated for:
- Oesophageal Cancer: Both early-stage and advanced oesophageal cancer.
- Barrett’s Oesophagus: With high-grade dysplasia that is at risk of progressing to cancer.
- Severe Oesophageal Stricture: That is refractory to other treatments.
- Oesophageal Perforation: In cases where the damage is severe.
- Achalasia: Severe cases where the oesophagus is significantly dilated and non-functional.
Types of Oesophagectomy
- Transhiatal Oesophagectomy (THE):
- Performed through incisions in the neck and abdomen, avoiding the thorax.
- Suitable for tumours located in the lower third of the oesophagus.
2. Transthoracic Oesophagectomy (TTE):
- Involves an incision in the chest (thoracotomy) along with an abdominal incision.
- Can be performed as an Ivor Lewis oesophagectomy (abdomen and right chest) or a three-incision oesophagectomy (abdomen, right chest, and neck).
3. Minimally Invasive Oesophagectomy (MIO):
- Uses laparoscopic and thoracoscopic techniques to minimise incision size.
- Can be performed transhiatally or transthoracically.
Surgical Procedure
1. Preoperative Preparation
- Assessment: Detailed medical history, physical examination, imaging studies (CT, PET, endoscopy) to determine the extent of the disease.
- Nutritional Support: Patients may require nutritional support preoperatively due to difficulty swallowing.
- Anaesthesia Evaluation: Comprehensive evaluation due to the complexity of the surgery.
2. Anaesthesia
- General anaesthesia is administered for the procedure.
3. Surgical Steps
A) Transhiatal Oesophagectomy (THE):
- Incisions: Incisions made in the neck and abdomen.
- Oesophagus Mobilisation: The oesophagus is mobilised through the abdominal and neck incisions.
- Resection: The affected portion of the oesophagus is resected.
- Reconstruction: The stomach is pulled up and connected to the remaining oesophagus in the neck.
B) Transthoracic Oesophagectomy (TTE):
- Incisions: Incisions made in the abdomen and chest (and neck for the three-incision approach).
- Oesophagus Mobilisation: The oesophagus is mobilised through the abdominal and thoracic incisions.
- Resection: The affected portion of the oesophagus is resected.
- Reconstruction: The stomach (or occasionally the colon) is used to reconstruct the oesophagus, typically anastomosed in the chest or neck.
- Chest Tube Insertion:
- Purpose: Chest tubes (thoracostomy tubes) are inserted to drain air, blood, or other fluids from the pleural space (the area between the lungs and the chest wall). This helps prevent complications such as pneumothorax (collapsed lung) and pleural effusion.
- Placement: Usually placed during surgery and removed once the drainage decreases and the lungs have fully expanded.
C) Minimally Invasive Oesophagectomy (MIO):
- Incisions: Small incisions for laparoscopic and thoracoscopic instruments.
- Oesophagus Mobilisation and Resection: Similar to open procedures but done with minimally invasive tools.
- Reconstruction: Performed similarly using minimally invasive techniques.
4. Postoperative Care
- ICU Monitoring: Patients are often monitored in the ICU immediately after surgery.
- Nutritional Support: Enteral feeding through a jejunostomy tube initially, transitioning to oral intake as tolerated.
- Pain Management: Analgesics and sometimes epidural analgesia for pain control.
- Respiratory Support: Incentive spirometry, chest physiotherapy to prevent complications like pneumonia.
- Monitoring for Complications: Including anastomotic leak, infections, and respiratory complications.
Complications
Potential complications of oesophagectomy include:
- Anastomotic Leak: Leakage from the site where the oesophagus is reconnected.
- Infection: Including pneumonia, wound infections, or sepsis.
- Respiratory Complications: Due to the proximity of the surgery to the lungs.
- Stricture Formation: At the site of the anastomosis, leading to swallowing difficulties.
- Chylothorax: Leakage of lymphatic fluid into the chest cavity.
- Gastroesophageal Reflux: Due to changes in the anatomy of the oesophagus and stomach.
Recovery and Follow-Up
- Hospital Stay: Typically 1-2 weeks, depending on the patient’s recovery.
- Nutritional Management: Gradual reintroduction of oral intake, starting with liquids and progressing to solids.
- Physical Therapy: To improve strength and respiratory function.
- Regular Follow-Up: With the surgical team and oncologist to monitor for recurrence of cancer and manage any long-term complications.
- Lifestyle Adjustments: Patients may need to make dietary changes, eat smaller meals more frequently, and avoid certain foods to manage symptoms of reflux and ensure adequate nutrition.
Conclusion
Oesophagectomy is a complex surgical procedure primarily used to treat oesophageal cancer and other severe oesophageal conditions. The choice of surgical approach depends on the location and extent of the disease, as well as the patient’s overall health. While the procedure carries significant risks and potential complications, it can be life-saving and offers a chance for cure or significant symptom relief.
References:
