Pacing: An Overview
Pacing is a treatment method used to manage various types of heart blocks and other cardiac arrhythmias by using a pacemaker to deliver electrical impulses to the heart. This ensures that the heart maintains an adequate rate and rhythm. Pacing can be temporary or permanent, depending on the patient’s condition.
Types of Pacing
- Temporary Pacing
- Permanent Pacing
1. Temporary Pacing
Indications:
- Acute management of severe bradycardia or heart block.
- Temporary support during and after cardiac surgery.
- As a bridge to permanent pacemaker implantation in emergency situations.
Methods:
- Transcutaneous Pacing: External pacemaker pads are placed on the chest and back, delivering electrical impulses through the skin.
- Transvenous Pacing: A pacing wire is inserted into a central vein (e.g., subclavian or femoral vein) and advanced into the right ventricle.
- Epicardial Pacing: Used during cardiac surgery, pacing wires are placed on the epicardial surface of the heart and can be accessed externally.
Advantages:
- Rapid setup in emergency situations.
- Useful for short-term management.
Disadvantages:
- Can be uncomfortable for the patient, especially transcutaneous pacing.
- Risk of infection with transvenous and epicardial pacing.
2. Permanent Pacing
Indications:
- Chronic symptomatic bradycardia (e.g., sinus node dysfunction).
- High-degree AV block (Mobitz Type II or third-degree AV block).
- Heart failure patients with dyssynchrony (Cardiac Resynchronisation Therapy, CRT).
- Some cases of atrial fibrillation with slow ventricular response.
Pacemaker Types:
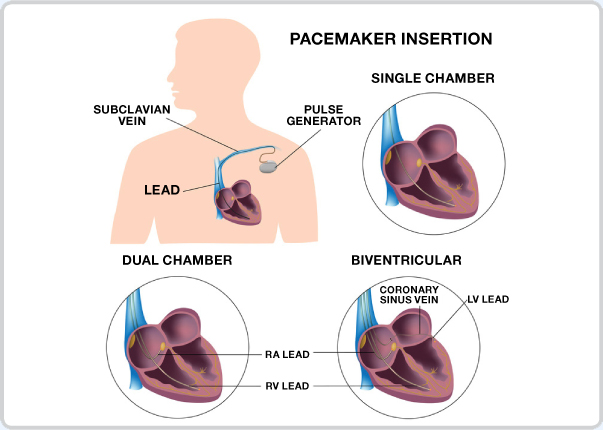
- Single-Chamber Pacemaker: One lead placed in either the right atrium or right ventricle.
- Dual-Chamber Pacemaker: Two leads, one in the right atrium and one in the right ventricle, allowing coordinated pacing.
- Biventricular Pacemaker (CRT): Leads placed in the right atrium, right ventricle, and through the coronary sinus to the left ventricle for resynchronisation in heart failure patients.
Pacemaker Implantation Procedure
Preparation:
- Pre-procedure evaluation including ECG, echocardiogram, and blood tests.
- Review of anticoagulation status and adjustment as needed.
Procedure:
- Typically performed under local anaesthesia with sedation.
- A small incision is made below the clavicle.
- Leads are inserted through a vein and positioned in the heart chambers under fluoroscopic guidance.
- The pacemaker device is implanted in a subcutaneous pocket created under the skin.
- Lead positions and device function are tested before the incision is closed.
Post-Procedure Care:
- Monitoring for complications such as lead displacement, infection, or haematoma.
- Programming the pacemaker to appropriate settings based on the patient’s needs.
- Regular follow-up for device interrogation and adjustment.
Complications of Pacing
- Infection: At the site of the pacemaker or leads.
- Lead Displacement: Leads can move from their intended positions.
- Device Malfunction: Battery depletion or technical issues with the device.
- Vascular Complications: Hematoma, thrombosis, or pneumothorax.
- Pacemaker Syndrome: Symptoms caused by inappropriate timing of atrial and ventricular contractions.
Follow-Up and Monitoring
Regular Follow-Up:
- Device checks typically every 3-12 months, depending on the type of pacemaker and patient condition.
- Remote monitoring options are available for some devices.
Device Interrogation:
- Ensures proper functioning of the pacemaker.
- Checks battery status and lead integrity.
- Allows for reprogramming of pacing parameters if needed.
Lifestyle Considerations:
- Avoiding strong magnetic fields and certain types of machinery that can interfere with pacemaker function.
- Patients should carry a pacemaker identification card.
Summary
Pacing is a vital treatment for managing heart blocks and certain arrhythmias, providing life-saving and quality-of-life-improving benefits. Temporary pacing serves as a critical bridge in acute settings, while permanent pacing offers long-term solutions for chronic conditions. Proper patient selection, implantation technique, and follow-up care are essential to maximise the benefits and minimise the risks associated with pacemakers.
