Pancreatitis is an inflammation of the pancreas, a gland located behind your stomach that plays a crucial role in digestion. The pancreas produces digestive enzymes that help break down food in the small intestine, as well as hormones like insulin and glucagon, which regulate blood sugar levels.
Functions of the Pancreas:
The pancreas has both exocrine and endocrine functions:
- Exocrine Function:
- Digestive Enzymes: The pancreas secretes digestive enzymes into the small intestine through the pancreatic duct. These enzymes include:
- Amylase: Breaks down carbohydrates into simple sugars.
- Lipase: Breaks down fats into fatty acids and glycerol.
- Proteases (including trypsin and chymotrypsin): Break down proteins into amino acids.
- Digestive Enzymes: The pancreas secretes digestive enzymes into the small intestine through the pancreatic duct. These enzymes include:
- Endocrine Function:
- Hormones: The pancreas releases hormones directly into the bloodstream to regulate blood sugar levels. These hormones include:
- Insulin: Lowers blood sugar levels by facilitating the uptake of glucose into cells.
- Glucagon: Raises blood sugar levels by stimulating the release of glucose from the liver.
- Somatostatin: Regulates the secretion of other hormones and slows down the digestive process.
- Hormones: The pancreas releases hormones directly into the bloodstream to regulate blood sugar levels. These hormones include:
Types of Pancreatitis:
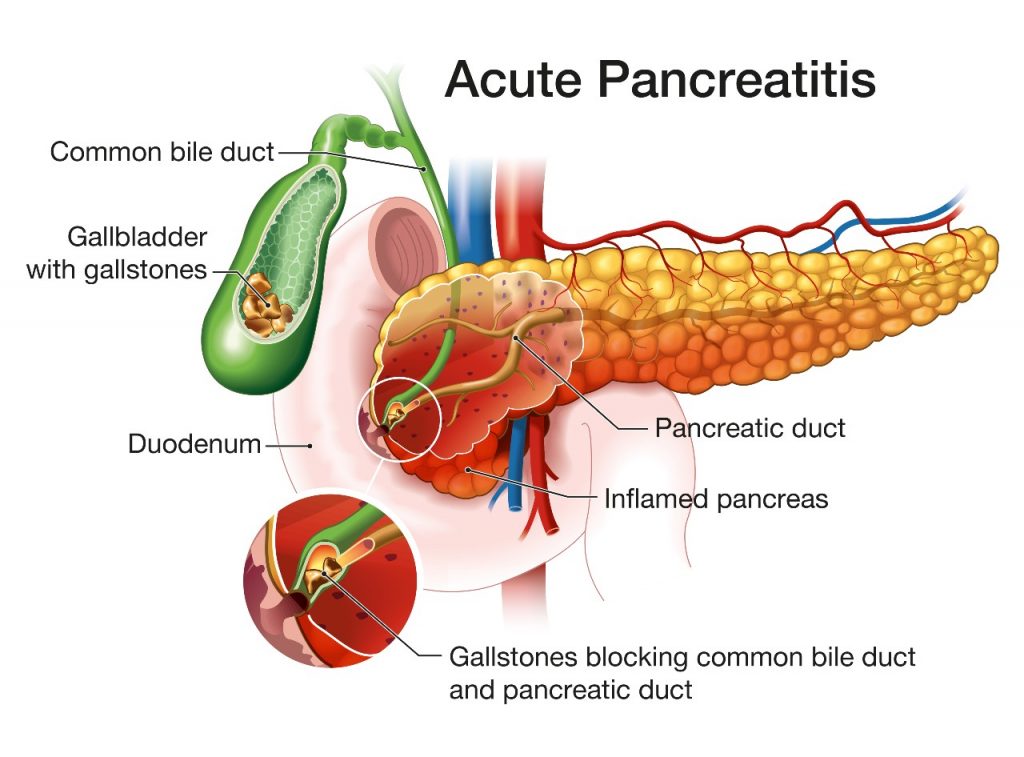
- Acute Pancreatitis: This is a sudden and severe inflammation of the pancreas. It typically comes on quickly and causes significant pain. Most cases of pancreatitis are acute.
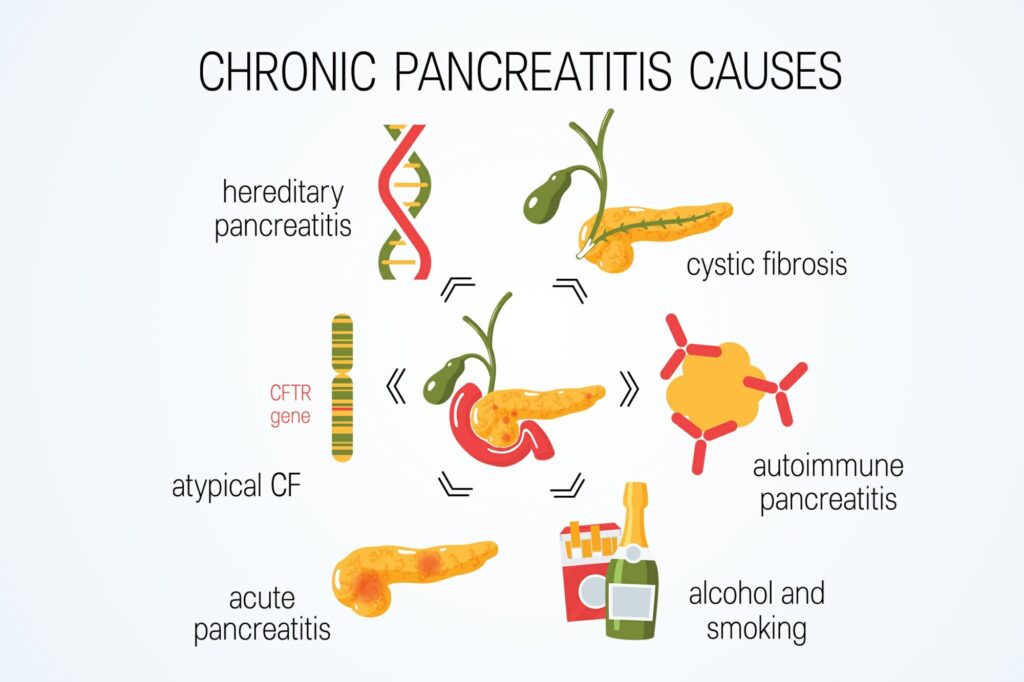
- Chronic Pancreatitis: This is a long-term condition characterised by repeated episodes of inflammation that can damage the pancreas permanently.
Causes:
- Gallstones: The most common cause of acute pancreatitis, gallstones can block the pancreatic duct.
- Alcohol Abuse: A significant cause of both acute and chronic pancreatitis due to prolonged heavy drinking.
- Medications: Certain drugs such as corticosteroids, azathioprine, and thiazide diuretics can induce pancreatitis.
- Infections: Viral infections like mumps, hepatitis, and Epstein-Barr virus.
- Trauma: Physical injury to the pancreas.
- Genetic Factors: Conditions like hereditary pancreatitis caused by genetic mutations.
- Autoimmune Conditions: The immune system mistakenly attacks the pancreas.
- Metabolic Disorders: Hypercalcaemia and hypertriglyceridaemia.
Symptoms:
Acute Pancreatitis:
- Severe Abdominal Pain: Typically in the upper abdomen, may radiate to the back, and worsens after eating.
- Nausea and Vomiting
- Fever
- Rapid Pulse
- Tenderness in the Abdomen
Chronic Pancreatitis:
- Persistent Abdominal Pain: Often severe and can be disabling.
- Weight Loss: Due to malabsorption of nutrients.
- Steatorrhoea: Oily, foul-smelling stools caused by fat malabsorption.
- Diabetes: Resulting from the destruction of insulin-producing cells.
Diagnosis:
- Blood Tests:
- Amylase and Lipase: Elevated levels are indicative of pancreatitis.
- Liver Function Tests: To check for gallstone-induced pancreatitis.
- Calcium and Triglycerides: To identify metabolic causes.
- Imaging Studies:
- Abdominal Ultrasound: To detect gallstones and assess pancreatic inflammation.
- CT Scan: Provides detailed images of the pancreas and surrounding structures.
- MRI/MRCP (Magnetic Resonance Cholangiopancreatography): To evaluate the pancreatic and bile ducts.
- Endoscopic Ultrasound (EUS): To obtain detailed images and perform fine-needle aspiration if necessary.
Management:
Acute Pancreatitis:
- Hospitalisation:
- Intravenous Fluids: To maintain hydration and support organ function.
- Pain Management: Using analgesics to control severe pain.
- Nutritional Support: Initially nil by mouth (NPO), followed by gradual reintroduction of oral intake. In severe cases, enteral feeding may be necessary.
- Antibiotics: Administered only if there is evidence of infection.
- Treatment of Underlying Causes:
- Gallstones: Removal through ERCP (Endoscopic Retrograde Cholangiopancreatography).
- Alcohol Cessation: Support for abstinence from alcohol.
Chronic Pancreatitis:
- Pain Management: Often requires long-term medication, nerve blocks, or surgical interventions.
- Enzyme Supplements: Pancreatic enzyme replacement therapy to aid digestion.
- Nutritional Support: Special diets low in fat and high in nutrients.
- Management of Diabetes: Insulin therapy or other medications.
- Lifestyle Changes: Abstaining from alcohol and smoking, maintaining a healthy diet.
Complications:
- Pseudocysts: Fluid collections that can become infected or rupture.
- Infection: Pancreatic necrosis can lead to severe infections.
- Diabetes: Due to the destruction of insulin-producing cells.
- Malnutrition: Resulting from poor absorption of nutrients.
- Pancreatic Cancer: Chronic inflammation increases the risk of developing pancreatic cancer.
Prognosis:
- Acute Pancreatitis: Most patients recover fully with appropriate treatment, though severe cases can be life-threatening.
- Chronic Pancreatitis: Requires long-term management to control symptoms and prevent complications. The prognosis depends on the underlying cause and adherence to treatment.
