Definition:
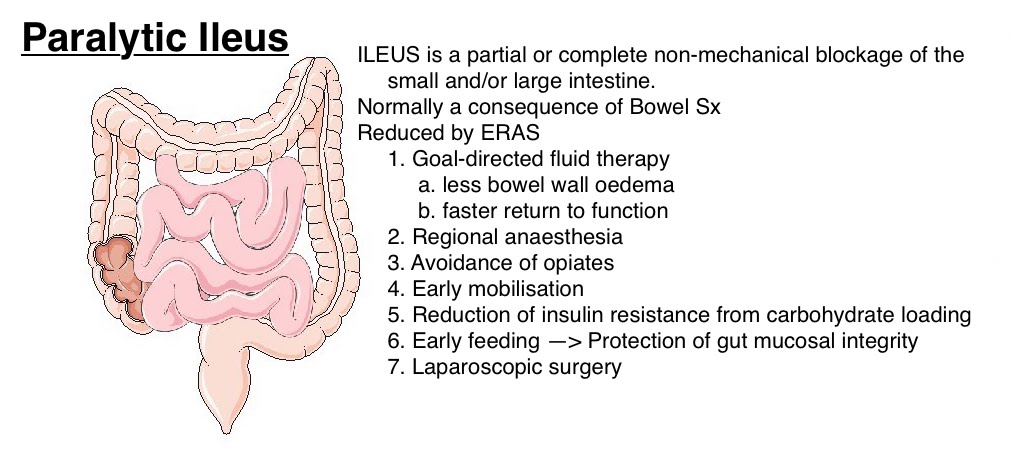
Paralytic ileus is a condition characterised by a temporary cessation of normal bowel motility and peristalsis without any mechanical obstruction. It results in the accumulation of gas and intestinal contents, leading to abdominal distension, pain, and other gastrointestinal symptoms.
Causes:
Paralytic ileus can result from various factors, including:
- Surgery: Abdominal or pelvic surgery, particularly when involving the intestines, is a common cause.
- Medications: Certain drugs, such as opioids, anticholinergics, and some antidepressants, can inhibit bowel motility.
- Infections: Intra-abdominal infections, peritonitis, and systemic infections can contribute to the development of ileus.
- Electrolyte Imbalances: Imbalances, particularly hypokalemia, hyponatremia, and hypomagnesemia, can affect bowel function.
- Medical Conditions: Conditions like pancreatitis, appendicitis, and severe illness or trauma can lead to paralytic ileus.
- Neurological Disorders: Spinal cord injuries and other neurological conditions can impair the nerve signals that control bowel movements.
Effects:
- Gastrointestinal Symptoms:
- Abdominal Distension: The most prominent effect, caused by the accumulation of gas and intestinal contents, leading to visible swelling and bloating.
- Abdominal Pain: Often crampy and diffuse, ranging from mild discomfort to severe pain.
- Nausea and Vomiting: Due to the accumulation of stomach and intestinal contents that cannot pass through the intestines, leading to backward flow.
- Bloating and Flatulence: Excess gas production and its retention in the intestines.
- Constipation: Severe reduction or absence of bowel movements and inability to pass gas.
- Metabolic and Nutritional Effects:
- Dehydration: Resulting from prolonged vomiting and the inability to absorb fluids normally through the digestive tract.
- Electrolyte Imbalances: Prolonged vomiting and lack of absorption can lead to imbalances such as hypokalaemia, hyponatraemia, and hypomagnesaemia, which can exacerbate the condition.
- Nutritional Deficiencies: Due to reduced food intake and absorption, patients may suffer from malnutrition and deficiencies in essential vitamins and minerals.
- Systemic Effects:
- Shock: Severe dehydration and electrolyte imbalances can lead to hypovolemic shock.
- Sepsis: If the ileus leads to bowel perforation, it can cause peritonitis and subsequent sepsis, a life-threatening systemic infection.
- Respiratory Complications:
- Aspiration Pneumonia: Vomiting and the subsequent risk of inhaling stomach contents into the lungs can lead to aspiration pneumonia.
- Psychological Effects:
- Anxiety and Stress: Chronic discomfort and the inability to predict bowel movements can lead to significant anxiety and stress.
- Depression: Long-term discomfort and lifestyle alterations due to paralytic ileus can contribute to depressive symptoms.
Complications:
- Bowel Perforation: Continued distension can compromise blood flow to the bowel wall, leading to ischaemia and eventual perforation.
- Peritonitis: Inflammation of the peritoneum due to bowel perforation, leading to severe abdominal pain, fever, and systemic infection.
- Chronic Ileus: In some cases, paralytic ileus can become chronic, requiring ongoing management and significantly impacting quality of life.
Diagnosis:
Diagnosis is primarily clinical, supported by imaging and laboratory tests:
- Physical Examination:
- Abdominal examination may reveal distension, reduced or absent bowel sounds, and tenderness.
2. Imaging Studies:
- Abdominal X-ray: Shows dilated loops of bowel with air-fluid levels, indicating a lack of movement.
- CT Scan: Provides detailed images to rule out mechanical obstruction and identify any underlying causes.
3. Laboratory Tests:
- Blood Tests: To check for electrolyte imbalances, infection, and other abnormalities.
Management:
Treatment of paralytic ileus focuses on addressing the underlying cause and relieving symptoms:
- Supportive Care:
- Bowel Rest: Nothing by mouth (NPO) to allow the bowel to rest.
- Intravenous Fluids: To maintain hydration and correct electrolyte imbalances.
- Nasogastric Decompression: A nasogastric tube may be inserted to relieve abdominal distension and prevent vomiting.
2. Medications:
- Prokinetic Agents: Drugs like metoclopramide may be used to stimulate bowel movements in some cases.
- Pain Management: Avoiding opioids if possible, as they can exacerbate ileus. Non-opioid analgesics are preferred.
3. Monitoring and Follow-Up:
- Regular monitoring of abdominal girth, bowel sounds, and overall clinical status.
- Gradual reintroduction of oral intake once bowel function starts to return.
Complications:
- Perforation: Risk of bowel perforation if the condition is severe or prolonged.
- Peritonitis: Inflammation of the abdominal lining, potentially leading to sepsis.
- Severe Dehydration and Electrolyte Imbalances: Due to prolonged vomiting and lack of oral intake.
Prognosis:
- The prognosis for paralytic ileus is generally good with appropriate management. However, the underlying cause must be treated to prevent recurrence.
- Recovery time varies depending on the cause and severity of the ileus.
