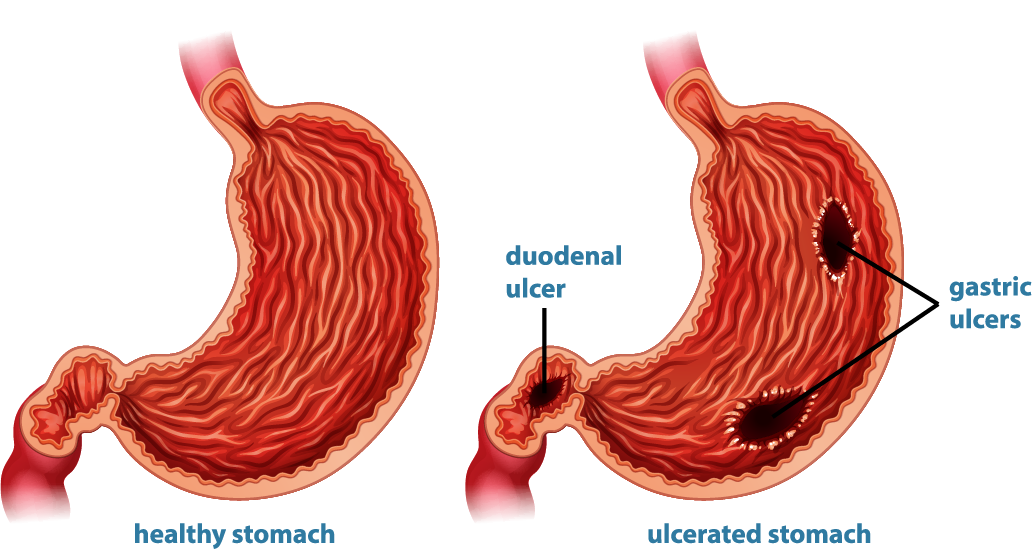
Peptic ulcers are open sores that develop on the inner lining of the stomach and the upper portion of the small intestine. When these ulcers occur in the stomach, they are called gastric ulcers, and when they occur in the first part of the small intestine (duodenum), they are called duodenal ulcers
These ulcers form when the protective mechanisms that normally shield the digestive tract from stomach acid are weakened or overwhelmed.
Causes:
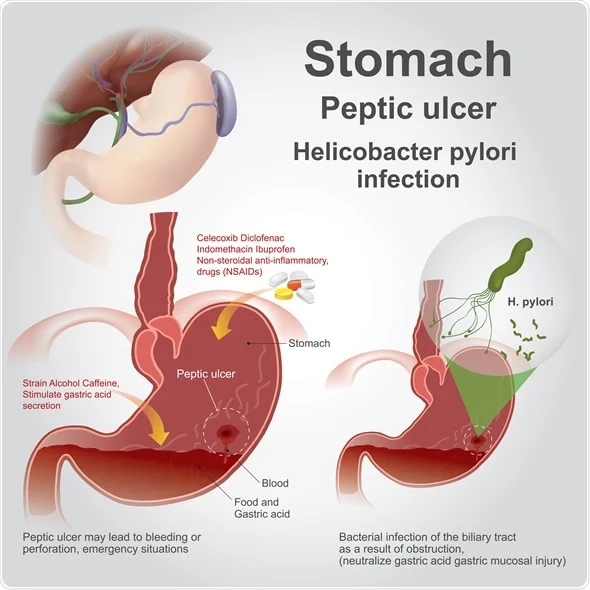
- Helicobacter pylori Infection:
- A significant cause of peptic ulcers, this bacterium damages the mucous coating that protects the lining of the stomach and duodenum, leading to sores.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs):
- Long-term use of NSAIDs such as ibuprofen and aspirin can irritate or inflame the lining of the stomach and small intestine, leading to ulcers.
- Excess Acid Production:
- Conditions such as Zollinger-Ellison syndrome can cause the stomach to produce too much acid, leading to ulcers.
- Other Factors:
- Smoking, excessive alcohol consumption, stress, and spicy foods can exacerbate the risk of developing ulcers, although they are not direct causes.
Symptoms:
Common Symptoms:
- Abdominal Pain: A burning or gnawing pain in the stomach area, which may be more noticeable on an empty stomach or at night.
- Bloating: Feeling of fullness or swelling in the abdomen.
- Heartburn: A burning sensation in the chest due to acid reflux.
- Nausea or Vomiting: Feeling sick or actually vomiting.
- Loss of Appetite and Weight Loss: Due to discomfort or pain after eating.
Severe Symptoms (indicative of complications):
- Vomiting Blood: Which may appear red or black.
- Black, Tarry Stools: Indicating bleeding in the stomach or duodenum.
Diagnosis:
- Medical History and Physical Examination:
- Discussing symptoms and history of NSAID use, alcohol consumption, and other risk factors.
- Endoscopy:
- An upper GI endoscopy allows direct visualisation of the ulcer and the possibility of taking a biopsy for further analysis.
- Tests for H. pylori:
- Urea Breath Test: Measures carbon dioxide in the breath after swallowing a urea solution.
- Stool Antigen Test: Detects the presence of H. pylori in the stool.
- Blood Test: Checks for antibodies against H. pylori, although this is less commonly used.
- Barium Swallow:
- A radiographic examination where the patient drinks a barium solution that coats the digestive tract, making ulcers visible on X-ray.
- Severe Abdominal Pain: That comes on suddenly and may signal a perforation or obstruction.
Management:
Medications:
- Antibiotics:
- Used to eradicate H. pylori infection. Common antibiotics include clarithromycin, amoxicillin, and metronidazole.
- Proton Pump Inhibitors (PPIs):
- Reduce stomach acid production, allowing the ulcer to heal. Examples include omeprazole, esomeprazole, and lansoprazole.
- H2-Receptor Antagonists:
- Also reduce acid production but are less potent than PPIs. Examples include ranitidine and famotidine.
- Antacids:
- Neutralise existing stomach acid and provide symptomatic relief. They do not promote healing but can alleviate discomfort.
- Cytoprotective Agents:
- Medications like sucralfate and misoprostol protect the stomach lining and help it heal.
Lifestyle and Dietary Changes:
- Avoid NSAIDs: If possible, find alternatives to NSAIDs for pain relief.
- Quit Smoking: Smoking increases stomach acid and impairs the protective lining of the stomach and duodenum.
- Limit Alcohol: Reduce or avoid alcohol to prevent further irritation of the stomach lining.
- Dietary Adjustments: Eat smaller, more frequent meals, avoid spicy and acidic foods, and reduce caffeine intake.
Surgical Treatment:
- Surgery is rarely needed but may be required in cases of complications such as perforation, bleeding that cannot be controlled with endoscopy, or obstruction. Procedures may include vagotomy (cutting the nerve that stimulates acid production) or partial gastrectomy (removal of part of the stomach).
Complications:
- Bleeding: Can lead to significant blood loss and anaemia.
- Perforation: An ulcer can create a hole in the stomach or duodenal wall, leading to peritonitis.
- Obstruction: Swelling and scarring from an ulcer can block the passage of food through the digestive tract.
Prognosis:
- With appropriate treatment, most peptic ulcers heal. However, recurrent ulcers can occur, especially if H. pylori infection is not completely eradicated or if NSAID use continues.
