Pressure controlled ventilation (PCV) is a type of mechanical ventilation where the ventilator delivers a breath to the patient’s lungs at a preset pressure for a set inspiratory time. Unlike volume-controlled ventilation, which delivers a specific volume of air, PCV delivers a breath until a certain pressure is reached.
The primary goal is to achieve adequate ventilation while minimising the risk of lung injury caused by high airway pressures.
How it Works
- Initiation: The ventilator starts the inspiratory phase based on a timed cycle or patient effort, depending on the mode of triggering.
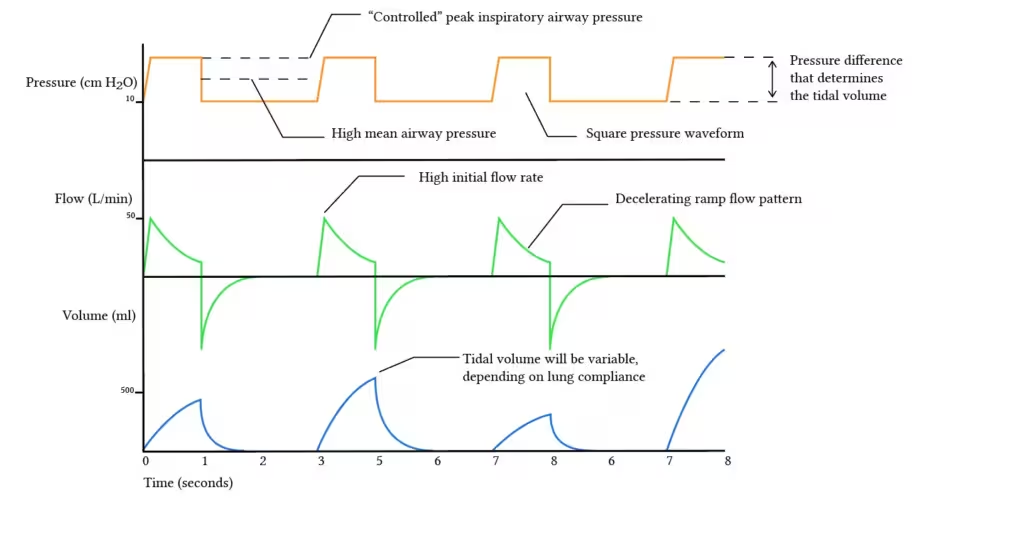
- Pressure Delivery: The ventilator rapidly achieves the preset inspiratory pressure and maintains this pressure for the duration of the inspiratory time.
- Plateau: The pressure is sustained throughout the inspiratory phase, allowing the lungs to fill with air.
- Exhalation: At the end of the inspiratory time, the ventilator allows the patient to passively exhale. Exhalation is usually passive and follows the natural elastic recoil of the lungs and chest wall.
Settings on a Ventilator for PCV
Preset Inspiratory Pressure: In PCV, the clinician sets a specific peak inspiratory pressure (PIP) that the ventilator will deliver with each breath. This pressure is maintained throughout the inspiratory phase.
Variable Tidal Volume: Unlike volume-controlled ventilation (VCV), where a fixed tidal volume is delivered with each breath, the tidal volume in PCV can vary. This variation depends on the patient’s lung compliance (the ability of the lung to expand) and airway resistance (the resistance to airflow within the airways).
Inspiratory Time: The inspiratory time (Ti) is the duration over which the preset pressure is applied. The clinician sets this time, and it influences the tidal volume delivered. Longer inspiratory times can increase tidal volume if lung compliance allows.
Respiratory Rate: The number of breaths per minute is also set by the clinician, ensuring that the patient receives adequate ventilation.
PEEP (positive end-expiratory pressure): A constant level of positive pressure applied at the end of exhalation to keep the airways open and improve oxygenation. PEEP is often used in conjunction with pressure support.
Indications for Use:
- Acute Respiratory Distress Syndrome (ARDS): PCV is often used in ARDS to protect the lungs from high pressures that can cause further damage.
- Patients with Poor Lung Compliance: Such as those with stiff lungs due to conditions like pulmonary fibrosis.
- High Risk of Barotrauma: To minimise the risk of lung injury due to high peak airway pressures.
Advantages:
- Control of Peak Pressure: By limiting the peak inspiratory pressure, PCV reduces the risk of barotrauma and volutrauma.
- Adaptability: PCV adapts to changes in lung compliance and airway resistance, which can be beneficial in dynamically changing respiratory conditions.
- Improved Oxygenation: Can be particularly useful in improving oxygenation in patients with severe hypoxemia.
Disadvantages:
- Variable Tidal Volumes: The variability in tidal volumes may lead to inconsistent minute ventilation, which requires close monitoring.
- Risk of Hypoventilation: If the set pressure is too low or if lung compliance is significantly reduced, it may result in inadequate ventilation.
- May not be suitable for all patients: PCV may not be appropriate for patients with severe airway obstruction or who require a guaranteed tidal volume.
Clinical Monitoring:
- Tidal Volume Monitoring: Continuous monitoring of tidal volumes is crucial to ensure adequate ventilation and adjust settings as needed.
- Arterial Blood Gases (ABGs): Regular ABG analysis helps monitor the patient’s oxygenation and ventilation status.
- Patient-Ventilator Synchrony: Ensuring that the patient’s spontaneous efforts are well-coordinated with the ventilator to prevent dessynchrony.
References:
- Intensive Care Society – ARDS Guideline.
- Provides comprehensive guidelines on the management of ARDS, including ventilation strategies like PCV.
- British Thoracic Society – Guidelines and Standards.
- Offers guidelines on respiratory care practices, including invasive ventilation methods such as PCV.
- MacIntyre, N. R., & Branson, R. D. (2009). Mechanical Ventilation. Elsevier Health Sciences.
- Covers various aspects of mechanical ventilation, including detailed explanations and clinical guidelines for PCV.
- Kacmarek, R. M., Stoller, J. K., & Heuer, A. J. (2016). Egan’s Fundamentals of Respiratory Care. Elsevier.
- A comprehensive resource on respiratory care, offering in-depth discussions on different ventilation modes, including Pressure-Controlled Ventilation (PCV).
