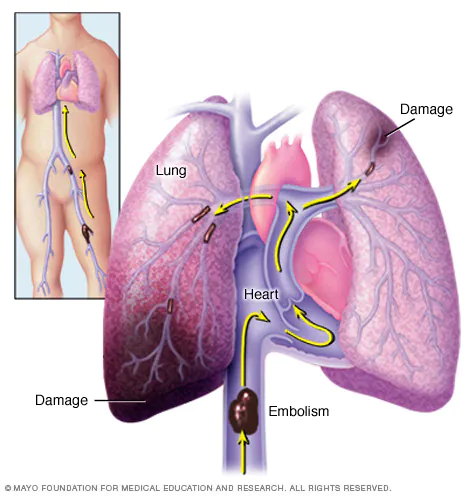
Pulmonary embolism (PE) is a condition where one or more arteries in the lungs become blocked by a blood clot. This clot typically originates from the deep veins in the legs, a condition known as deep vein thrombosis (DVT), and travels through the bloodstream to the lungs.
Causes
The primary cause of PE is the formation of blood clots in the deep veins of the legs (DVT). Several factors can contribute to the development of these clots, including:
- Immobilisation: Long periods of inactivity, such as during prolonged bed rest or long-haul flights, can slow blood flow and increase the risk of clot formation.
- Surgery: Major surgery, particularly orthopaedic procedures, can increase the risk of clot formation due to injury to blood vessels and prolonged immobility.
- Medical Conditions: Conditions such as cancer, heart disease, and genetic clotting disorders can increase the risk of DVT and PE.
- Hormonal Factors: Use of oral contraceptives, hormone replacement therapy, and pregnancy can increase clotting risk due to hormonal changes.
- Trauma: Injuries to the legs or pelvis can result in blood clots.
Signs & Symptoms
The symptoms of PE can vary greatly, depending on the size of the clot and the portion of the lung affected. Common signs and symptoms include:
- Shortness of Breath: Sudden and unexplained difficulty breathing.
- Chest Pain: Sharp or stabbing pain that may worsen with deep breaths or coughing.
- Cough: Possibly with bloody or blood-streaked sputum.
- Rapid Heart Rate: Tachycardia as the heart works harder to pump blood through obstructed pulmonary arteries.
- Light-headedness or Dizziness: Can occur due to decreased oxygenation.
- Sweating and Fever: May accompany other symptoms.
Pathophysiology
The pathophysiological mechanisms of PE involve several stages:
- Clot Formation: Blood clots form in the deep veins of the legs (DVT) due to factors like venous stasis, endothelial injury, and hypercoagulability.
- Clot Dislodgement and Embolisation: Portions of the clot break off and travel through the bloodstream to the lungs.
- Lodgement in Pulmonary Arteries: The emboli lodge in the pulmonary arteries, blocking blood flow.
- Hemodynamic and Respiratory Effects:
- Reduced Blood Flow: Leads to increased pulmonary vascular resistance and pressure.
- Impaired Gas Exchange: Reduced blood flow to the alveoli leads to a ventilation-perfusion mismatch, causing hypoxaemia.
- Right Ventricular Strain: The increased resistance puts a strain on the right ventricle, potentially leading to right heart failure.
Diagnosis
Diagnosing PE involves a combination of clinical assessment, imaging, and laboratory tests:
- Clinical Assessment:
- Detailed medical history and physical examination to assess risk factors and symptoms.
- Imaging:
- CT Pulmonary Angiography (CTPA): The gold standard for diagnosing PE, providing detailed images of blood vessels in the lungs.
- Ventilation-Perfusion (V/Q) Scan: Used when CTPA is contraindicated; it detects mismatched areas of ventilation and perfusion in the lungs.
- Doppler Ultrasound: To detect DVT in the legs, which often coexists with PE.
- Laboratory Tests:
- D-Dimer Test: Elevated levels suggest the presence of an abnormal blood clot; however, it is non-specific.
- Arterial Blood Gas (ABG): To assess oxygenation and gas exchange.
Management
The management of PE involves immediate treatment to dissolve the clot and prevent further clot formation:
- Anticoagulation Therapy:
- Initial Treatment: Heparin (unfractionated or low molecular weight heparin) to prevent further clotting.
- Long-term Treatment: Oral anticoagulants such as warfarin, or newer direct oral anticoagulants (DOACs) like rivaroxaban or apixaban.
- Thrombolytic Therapy:
- For severe cases with hemodynamic instability, thrombolytics (clot-dissolving drugs) like alteplase may be used.
- Surgical and Interventional Procedures:
- Embolectomy: Surgical removal of the embolus in life-threatening cases.
- Inferior Vena Cava (IVC) Filter: Placed in the IVC to prevent future clots from reaching the lungs, typically used in patients who cannot take anticoagulants.
- Supportive Care:
- Oxygen therapy to maintain adequate oxygenation.
- Fluids and medications to support blood pressure and heart function if necessary.
Prevention
- Lifestyle Modifications: Regular exercise, maintaining a healthy weight, and avoiding prolonged immobility.
- Prophylactic Anticoagulation: In high-risk patients, such as those undergoing major surgery or hospitalised for serious illness.
- Compression Stockings: To prevent DVT in at-risk individuals.
