Supraventricular Tachycardia (SVT) refers to a set of heart rhythm disorders characterised by an abnormally fast heart rate originating from the atria or other structures above the ventricles. In SVT, the heart rate typically exceeds 100 beats per minute and may reach 150-250 beats per minute.
Pathophysiology – Normally impulse travels in one direction i.e atria to ventricles.
normally impulse don’t travel back from ventricles to atria. However in most cases of SVT it is caused by electric signals re-entering the atria from the ventricles.
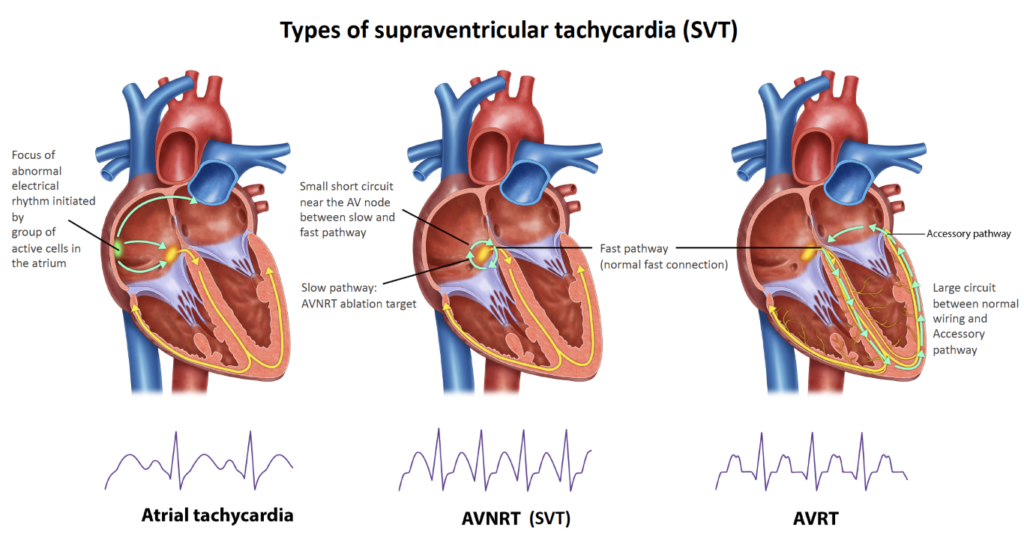
Types of SVT (by source of electric signal)
- Atrioventricular Nodal Reentrant Tachycardia (AVNRT): The most common type of SVT, where the electrical signals travel in a circular movement within the atrioventricular node due to the presence of more than one pathway. ( when the re-entry point is back through the AV node )
- Atrioventricular Reciprocating Tachycardia (AVRT): Associated with the presence of an additional electrical pathway between the atria and ventricles that can cause episodes of rapid heart rate. ( DETLA wave and short PR interval- premature entry from the accessory pathway) Wolff-Parkinson-White (WPW) Syndrome: A type of AVRT caused by an additional electrical pathway (accessory pathway) between the atria and the ventricles, leading to episodes of tachycardia. WPW is often identified by a characteristic pattern on an ECG known as a delta wave.
- Atrial Tachycardia: Originates from an abnormal focus within the atria and is less dependent on the atrioventricular node.
Causes
Several factors can contribute to SVT episodes:
- Underlying Heart Disease: Conditions like coronary artery disease or heart valve problems can create areas in the atria prone to abnormal electrical firing.
- Electrolyte Imbalances: Abnormal levels of electrolytes like potassium or magnesium can disrupt the electrical signals in the heart.
- Stress or Anxiety: Emotional stress can sometimes trigger SVT episodes in susceptible individuals.
- Certain Medications or Stimulants: Excessive caffeine intake, decongestants, or some medications can act as stimulants and trigger SVT.
- Inherited Conditions: WPW syndrome is an example of an inherited condition that can predispose someone to SVT.
ECG Findings :
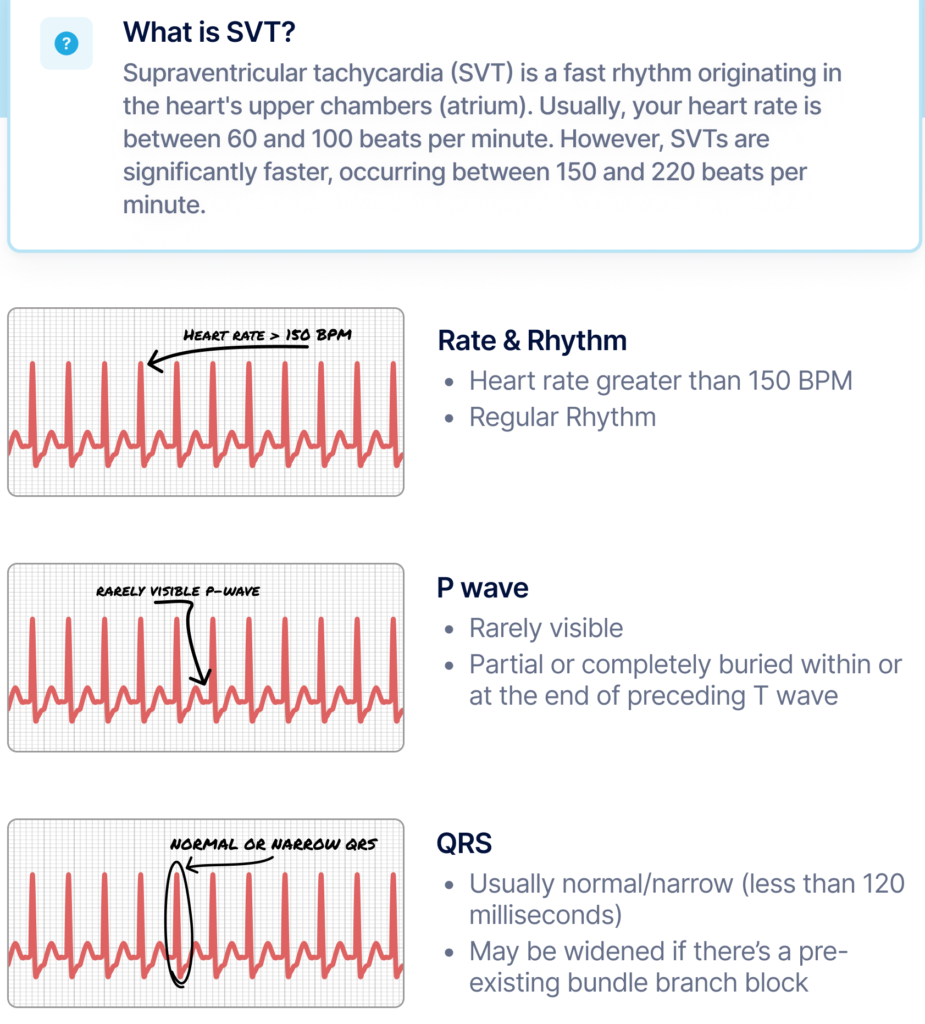
Heart Rate: The most prominent feature is a rapid heart rate, often 140 -250 beats per minute (bpm).
P Waves: These can be:
- Absent: In some types of SVT, the P waves might be hidden within the QRS complexes due to the rapid heart rate
- Wolff-Parkinson-White (WPW) Syndrome: A delta wave, a small deflection before the QRS complex, might be present along with abnormal P waves.
- Short P-R interval (<120 ms) due to the presence of an accessory pathway.
Treatment and Management
1. Acute Management
- Vagal Manoeuvres: Techniques such as the Valsalva manoeuvre and carotid sinus massage can help terminate SVT episodes by stimulating the vagus nerve, which can slow the heart rate.
- Valsalva Manoeuvre: Involves taking a deep breath and then trying to exhale forcefully with the mouth closed and nostrils pinched shut. This increases pressure in the chest and stimulates the vagus nerve, which can interrupt the reentrant circuit causing the tachycardia.
- Carotid Sinus Massage: Gently massaging the carotid artery in the neck can also stimulate the vagus nerve. This should only be performed by a healthcare professional due to the risk of stroke from dislodging plaque in the carotid artery.
- Adenosine administration: An effective drug that can quickly stop an SVT episode by temporarily blocking the AV node’s conduction & accessory pathway during SVT and reset back to sinus rhythm. The half life of Adenosine is less then 10 seconds, meaning it metabolised very quickly.
- 6 mg: This is the first-line dose of adenosine administered as a rapid intravenous (IV) bolus injection over 1 to 2 seconds. A rapid flush of saline solution (usually 20 mL) follows the injection to ensure complete delivery of the medication.
- If the initial 6 mg dose fails to terminate the SVT within 1 to 2 minutes, a second dose of 12 mg can be administered following the same rapid IV bolus and saline flush procedure.
- In rare cases, a third dose of 12 mg might be considered, but this should only be done under the supervision of a healthcare professional and with careful monitoring.
- Electrical Cardioversion: This is used in cases where SVT is refractory to vagal maneuvers and medication. It involves delivering a synchronised electrical shock to the heart to restore a normal rhythm. Electrical cardioversion is typically performed in a controlled hospital setting under sedation.
2. Long-term Management
- Beta-blockers and calcium channel blockers: To control heart rate and prevent recurrent episodes.
- Antiarrhythmic drugs: Such as flecainide or amiodarone, particularly in more complex cases.
3. Invasive Interventions
- Catheter Ablation: Recommended for recurrent SVT that doesn’t respond to medical treatments. This procedure involves destroying the small area of heart tissue that’s causing the rapid heartbeats.
- Pacemaker Implantation: In select cases, especially in patients with AV node dysfunction.
