Toxic mega-colon is a severe, life-threatening complication of inflammatory bowel disease (IBD) such as ulcerative colitis and Crohn’s disease, or infectious colitis (e.g., Clostridioides difficile infection). It is characterised by rapid dilation of the colon, systemic toxicity, and potential perforation.
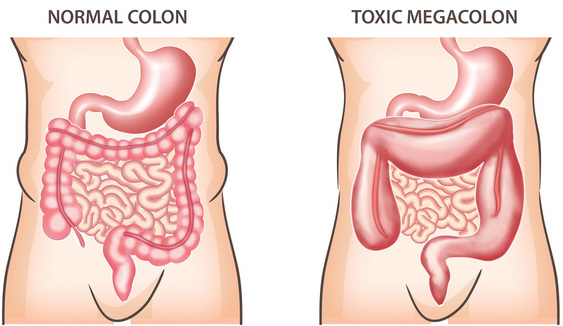
Pathophysiology: Toxic mega-colon occurs when severe inflammation extends into the muscle layers of the colon, leading to paralysis of the colon (colonic ileus) and distension. The dilated colon is at risk of perforation, which can lead to peritonitis and sepsis.
- Inflammation:
- Inflammatory mediators cause severe mucosal damage and ulceration.
- The inflammation extends to the muscularis and serosal layers.
2. Colonic Ileus:
- The inflammation leads to paralysis of the colonic muscles.
- This results in the accumulation of gas and stool, causing distension.
3. Dilation and Risk of Perforation:
- Continued distension can compromise blood flow to the colon, increasing the risk of ischaemia and perforation.
- Perforation can lead to peritonitis, sepsis, and potentially death.
Clinical Features:
- Severe Abdominal Pain: Often continuous and diffuse.
- Distension: Abdominal bloating and visible swelling.
- Fever: High fever indicating systemic infection.
- Tachycardia: Rapid heart rate.
- Shock: Low blood pressure and signs of systemic toxicity.
- Altered Mental Status: Confusion or lethargy.
- Diarrhoea: Often severe, and may be bloody.
Diagnosis: Diagnosis of toxic megacolon is clinical, supported by imaging and laboratory findings.
- Clinical Criteria (according to the criteria of Jalan et al.):
- Radiographic evidence of colonic distension (diameter > 6 cm).
- Any three of the following: fever (>38.6°C), heart rate >120 beats/min, white blood cell count >10,500/microlitre, anaemia.
- Plus, any one of the following: dehydration, altered mental status, electrolyte disturbances, or hypotension.
- Imaging:
- Abdominal X-ray: Shows colonic dilation and possibly air-fluid levels.
- CT Scan: Provides detailed images and helps identify complications like perforation.
- Laboratory Tests:
- Complete Blood Count (CBC): To check for elevated white blood cells.
- Electrolyte Panel: To identify imbalances.
- Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Management:
Management of toxic mega-colon involves both medical and surgical interventions.
- Medical Management:
- Resuscitation: Intravenous fluids to correct dehydration and electrolyte imbalances.
- Antibiotics: Broad-spectrum antibiotics to treat underlying infection and prevent sepsis.
- Bowel Rest: Nothing by mouth (NPO) to reduce bowel activity.
- Nasogastric Decompression: A nasogastric tube may be inserted to relieve abdominal distension.
- Medications: Corticosteroids or other anti-inflammatory drugs to reduce inflammation. In cases of C. difficile infection, appropriate antibiotics (e.g., vancomycin or metronidazole) are used.
- Surgical Management:
- Indications for Surgery: Surgery is indicated if there is no improvement with medical management within 24-48 hours, or if complications such as perforation, severe bleeding, or peritonitis occur.
- Types of Surgery:
- Subtotal Colectomy with Ileostomy: Removal of the colon with the creation of an ileostomy. This is the most common surgical procedure for toxic megacolon.
- Segmental Resection: In select cases, only the affected segment of the colon is removed.
- Total Proctocolectomy: Removal of the colon and rectum, usually considered if there is significant involvement of the rectum or as a definitive procedure for ulcerative colitis.
Prognosis: The prognosis of toxic megacolon depends on the promptness of treatment and the presence of complications. Early recognition and aggressive management are crucial to improving outcomes. The mortality rate increases significantly if perforation and sepsis occur.
References:
