Heart Blocks: Types, Causes, and Treatments
Heart blocks, or atrioventricular (AV) blocks, refer to disruptions in the electrical conduction system of the heart, impairing the transmission of impulses from the atria to the ventricles. These blocks are categorised into first-degree, second-degree (Mobitz type I and type II), and third-degree (complete) heart blocks. Each type has distinct ECG characteristics, causes, and treatment approaches.
1. First-Degree AV Block
Definition:
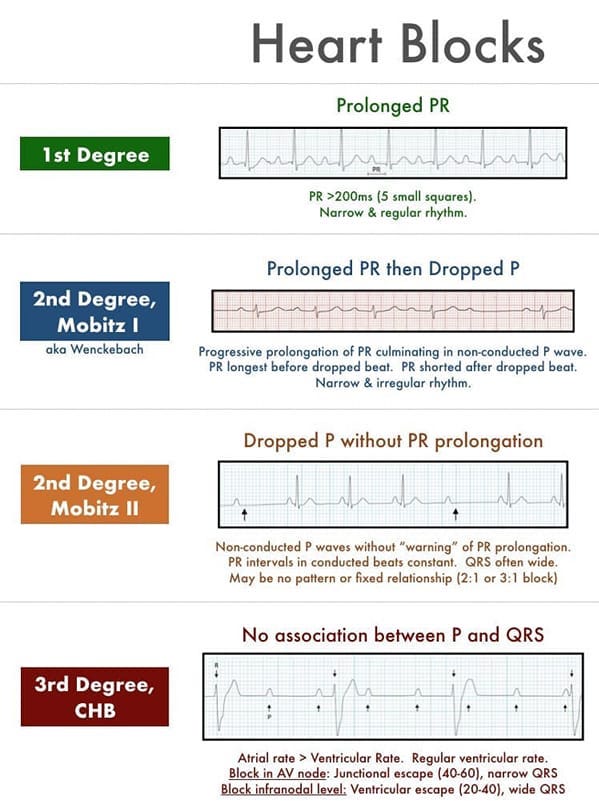
- A first-degree AV block is characterised by a prolonged PR interval on the ECG (greater than 200 milliseconds), with all atrial impulses being conducted to the ventricles.
ECG Features:
- PR interval > 200 ms
- Every P wave is followed by a QRS complex
- Regular rhythm
Causes:
- Increased Vagal Tone: Common in athletes due to high vagal tone.
- Medications: Beta-blockers, calcium channel blockers, digoxin.
- Myocardial Infarction: Especially inferior MI.
- Electrolyte Imbalances: Hyperkalemia, hypokalemia.
- Degenerative Changes: Aging-related fibrosis or sclerosis of the conduction system.
Clinical Significance:
- Often asymptomatic and discovered incidentally.
- Usually does not require treatment unless associated with symptoms or other conditions.
Treatment:
- Asymptomatic: Typically no treatment is needed; just regular monitoring.
- Symptomatic: Adjust or discontinue medications contributing to the block, treat underlying electrolyte imbalances, and manage myocardial infarction appropriately.
2. Second-Degree AV Block
Second-degree AV block involves intermittent failure of atrial impulses to be conducted to the ventricles and is subdivided into Mobitz type I (Wenckebach) and Mobitz type II.
Mobitz Type I (Wenckebach):
Definition:
- Progressive lengthening of the PR interval until a P wave is not followed by a QRS complex, with the cycle then repeating.
ECG Features:
- Progressive PR interval prolongation until a beat is dropped.
- Irregular rhythm due to dropped beats.
Causes:
- Increased Vagal Tone: Seen in athletes and during sleep.
- Medications: Digitalis, beta-blockers, calcium channel blockers.
- Myocardial Infarction: Particularly inferior MI.
- Infectious and Inflammatory Conditions: Lyme disease, myocarditis.
Clinical Significance:
- Often benign and can occur in healthy individuals.
- May cause symptoms like dizziness or syncope if significant.
Treatment:
- Asymptomatic: No treatment needed; periodic monitoring.
- Symptomatic: Discontinue or adjust medications, use atropine if needed for acute symptomatic episodes, and consider a pacemaker in severe cases.
Mobitz Type II:
Definition:
- Constant PR intervals with occasional dropped QRS complexes without progressive lengthening of the PR interval.
ECG Features:
- Fixed PR intervals with sudden dropped QRS complexes.
- The ratio of P waves to QRS complexes can vary (e.g., 2:1, 3:1).
Causes:
- Anterior Myocardial Infarction: Affecting the conduction system.
- Structural Heart Disease: Fibrosis, cardiomyopathy.
- Inflammatory Conditions: Myocarditis, sarcoidosis.
- Degenerative Disease: Aging-related conduction system degeneration.
Clinical Significance:
- More serious than Mobitz type I.
- Can lead to complete heart block.
- Often symptomatic, causing fatigue, dizziness, and syncope.
Treatment:
- Immediate: Temporary pacing if symptomatic or haemodynamically unstable.
- Long-term: Permanent pacemaker insertion due to the high risk of progression to complete heart block.
3. Third-Degree AV Block (Complete Heart Block)
Definition:
- A complete failure of atrial impulses to be conducted to the ventricles, resulting in independent atrial and ventricular activity.
ECG Features:
- No relationship between P waves and QRS complexes (AV dissociation).
- Regular P waves and regular QRS complexes, but at different rates.
- Atrial rate is faster than the ventricular rate.
- Ventricular escape rhythms can be narrow or broad QRS complexes, depending on the escape focus.
Causes:
- Congenital Heart Disease: Congenital complete heart block.
- Myocardial Infarction: Especially in the context of ischeamic heart disease.
- Cardiac Surgery: Post-surgical complication affecting the conduction system.
- Inflammatory and Infiltrative Diseases: Myocarditis, sarcoidosis, amyloidosis.
- Medications and Toxins: Beta-blockers, calcium channel blockers, digoxin, certain anti-arrhythmic drugs.
- Degenerative Changes: Idiopathic fibrosis, Lev’s disease.
Clinical Significance:
- Symptoms include fatigue, dizziness, syncope, and possibly heart failure.
- A medical emergency requiring immediate intervention.
Treatment:
- Acute Management: Immediate temporary pacing if symptomatic or haemodynamically unstable.
- Chronic Management: Permanent pacemaker insertion is generally required.
- Address Reversible Causes: Adjust medications, treat myocardial infarction, manage underlying inflammatory or infiltrative conditions.
Summary
Heart blocks are categorised into first-degree, second-degree (Mobitz type I and II), and third-degree (complete) based on the severity and pattern of the conduction impairment. Each type has distinct ECG characteristics, causes, and treatment strategies. Understanding these differences is crucial for accurate diagnosis and effective management. Treatment ranges from monitoring and addressing underlying causes to the insertion of a pacemaker for more severe blocks. Proper interpretation and intervention can significantly improve patient outcomes in individuals with heart blocks.
