Ventilator-associated pneumonia (VAP) is a type of hospital-acquired pneumonia that develops in patients who have been on mechanical ventilation through an endotracheal or tracheostomy tube for at least 48 hours. It is a significant cause of morbidity and mortality in the intensive care unit (ICU).
Causes
VAP is primarily caused by bacterial infections, with common pathogens including:
- Gram-negative bacteria:
- Pseudomonas aeruginosa
- Escherichia coli
- Klebsiella pneumoniae
- Acinetobacter spp.
- Gram-positive bacteria:
- Staphylococcus aureus (including MRSA)
- Other pathogens:
- Enterobacteriaceae
- Legionella pneumophila
Risk Factors
- Prolonged mechanical ventilation
- Aspiration of oropharyngeal secretions
- Use of sedatives and muscle relaxants
- Prior antibiotic therapy
- Underlying chronic lung disease
- Immunosuppression
Signs & Symptoms
- Fever and chills
- Increased respiratory secretions, often purulent
- Worsening gas exchange (hypoxaemia)
- Increased respiratory rate
- Increased white blood cell count
- New or progressive infiltrates on chest X-ray
Pathophysiology
- Colonisation and Aspiration:
- Endotracheal tubes bypass the body’s natural defence mechanisms, allowing direct entry of pathogens.
- Aspiration of contaminated secretions from the oropharynx or stomach can introduce bacteria into the lower respiratory tract.
- Biofilm Formation:
- Pathogens form biofilms on the surface of the endotracheal tube, which protect them from antibiotics and immune responses.
- Inflammatory Response:
- The presence of bacteria triggers an intense inflammatory response in the lungs.
- Inflammatory cells and fluid accumulate in the alveoli, leading to impaired gas exchange.
Diagnosis
Diagnosis of VAP involves a combination of clinical, radiographic, and microbiological criteria:
- Clinical Criteria:
- New or progressive infiltrate on chest X-ray
- At least two of the following: fever, leukocytosis or leukopenia, purulent tracheal secretions.
- Microbiological Testing:
- Tracheal aspirate cultures
- Bronchoalveolar lavage (BAL) cultures
- Protected specimen brush (PSB) cultures
- Radiographic Imaging:
- Chest X-ray or CT scan showing new or worsening infiltrates.
Management
- Preventive Measures:
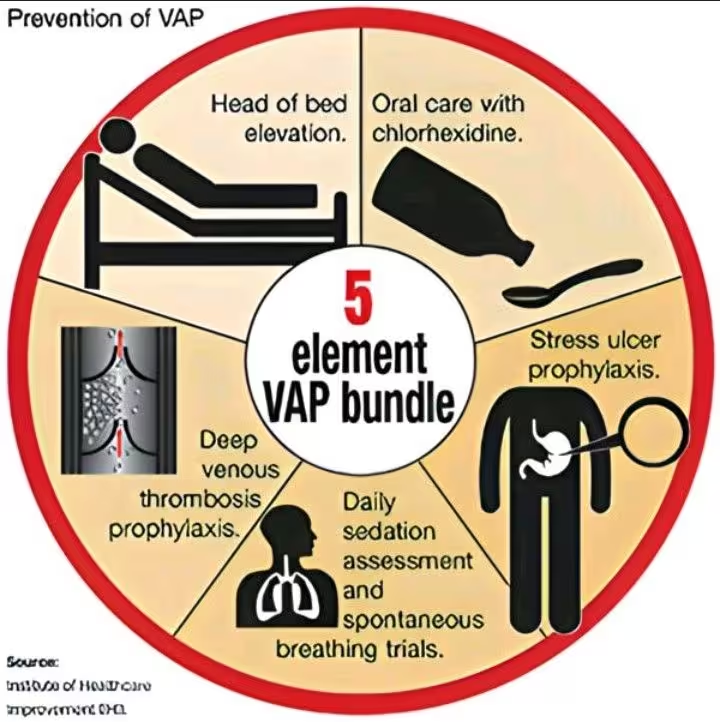
- Ventilator Bundle:
- Elevating the head of the bed to 30-45 degrees.
- Daily sedation vacations and assessment of readiness to extubate.
- Peptic ulcer disease prophylaxis.
- Deep venous thrombosis prophylaxis.
- Daily oral care with chlorhexidine.
- Hand Hygiene: Strict adherence to hand hygiene protocols.
- Aspiration Precautions: Proper cuff management and subglottic suctioning.
- Ventilator Bundle:
- Empirical Antibiotic Therapy:
- Initiate broad-spectrum antibiotics based on local antibiogram and suspected pathogens.
- Common choices include:
- Anti-pseudomonal beta-lactams: Piperacillin-tazobactam, cefepime.
- Carbapenems: Meropenem, imipenem.
- MRSA coverage: Vancomycin or linezolid.
- De-escalate therapy based on culture results and clinical response.
- Supportive Care:
- Continued mechanical ventilation with appropriate settings.
- Supplemental oxygen to maintain adequate oxygenation.
- Fluid management to ensure hemodynamic stability.
- Monitoring and Follow-Up:
- Regular assessment of respiratory status, oxygenation, and response to treatment.
- Adjust antibiotic therapy based on microbiological results and patient progress.
Outcomes
- Early identification and appropriate management of VAP are crucial to improve outcomes.
- Prolonged mechanical ventilation and ICU stay are associated with higher morbidity and mortality.
- Implementation of preventive measures can significantly reduce the incidence of VAP.
